| A 78 year-old woman presented with two years of unsteady gait and difficulty using her hands. Her exam was notable for prominent apraxia of both upper extremities and cortical sensory loss (i.e., agraphesthesia, astereognosis). She had increased tone in both legs and a slow shuffling gait. |
![]()
![]()
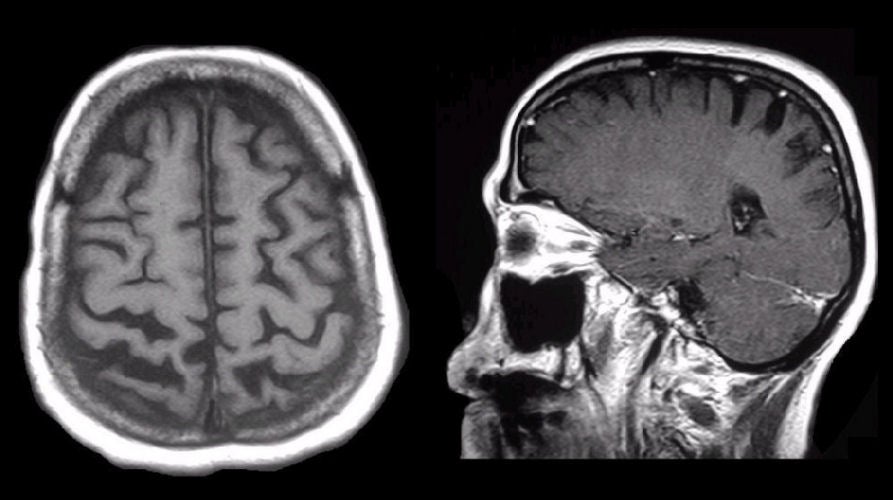
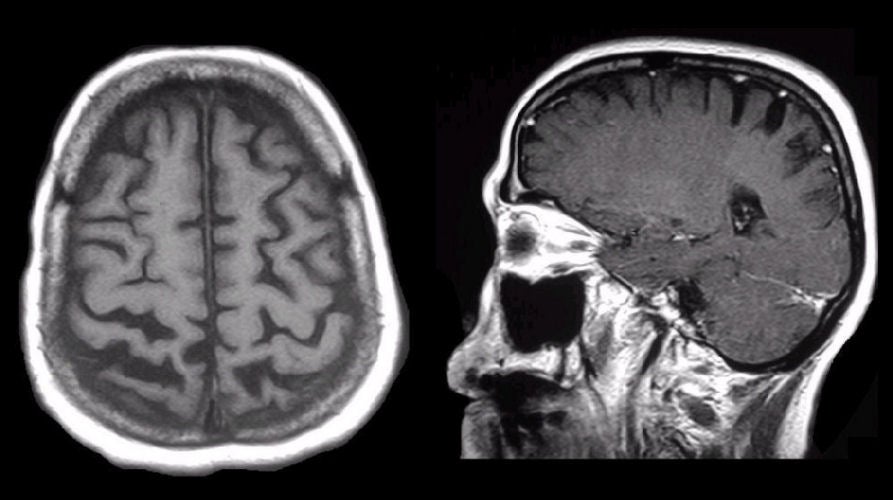
| Corticobasal Ganglionic Degeneration: (Left) T1-weighted
axial MRI; (Right) T1-weighted sagittal MRI.
Note the prominent atrophy in the parietal lobes bilaterally, with widening of
the adjacent sulci. In addition, note the enlargement and slight asymmetry of
the superior frontal sulci, the left being slightly larger than the right side.
This patient has corticobasal ganglionic degeneration (CBGD), a rare degenerative disorder wherein the cortex (usually the parietal lobes most prominently) is affected, along with the basal ganglia. Patients often present with prominent cortical sensory loss and apraxia. In severe cases, patients display the "alien hand" syndrome, whereby their hand feels disconnected from the rest of their body. Dysfunction of the basal ganglia results in features of Parkinsonism, including increased tone, bradykinesia, and gait disturbance. However, in contrast to Parkinson's Disease, levodopa and similar drugs are ineffective. CBGD has significant overlap with other rare neurodegenerative disorders, including frontotemporal dementia, primary progressive aphasia (PPA), Pick's disease and progressive supranuclear palsy (PSP). |
Revised
11/27/06
Copyrighted 2006. David C Preston