|
A 55 year-old man developed progressive pain, weakness and paresthesias of the legs while walking or standing. Only sitting would relieve the symptoms. His neurological exam was normal other than depressed ankle reflexes. |
![]()
![]()
![]()
![]()
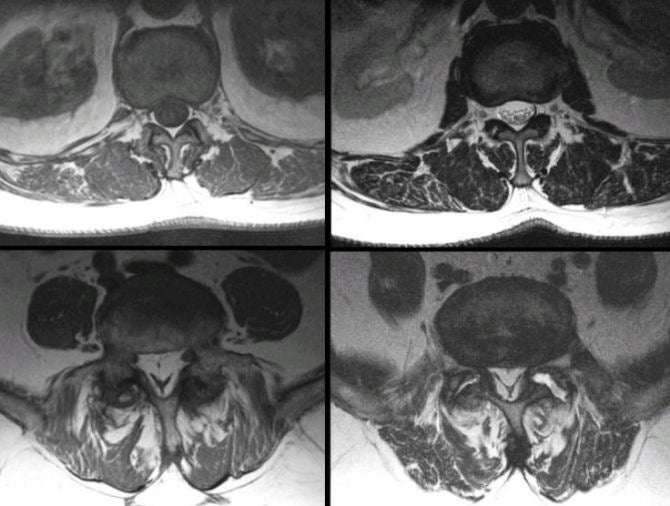
| Epidural Lipomatosis: (Left
Top) T1-weighted axial MRI at the L2-L3 level; (Left Bottom)
T2-weighted axial MRI at the L2-L3 level; (Right Top) T1-weighted
axial MRI at the L5-S1 level; (Right Bottom) T2-weighted axial MRI
at the L5-S1 level. The amount of epidural fat is normal at the
L2-L3 level, in contrast with the increased amount of epidural fat
seen at the L5-S1
level. Also note that the thecal sac maintains its typical oval shape at
the L2-L3 level, in contrast with the L5-S1 level, where it has been markedly compressed into a "stellate"
shape. Epidural lipomatosis refers to an abnormal accumulation of fat in the epidural space within the spine, which generally occurs in the lumbar and sacral regions. It is most often seen in the context of corticosteroid therapy, endocrinopathies (e.g. ectopic ACTH secretion), or significant obesity. Epidural steroid injections have also been implicated as an etiologic factor. Most patients present with back pain and lower extremity weakness, similar to patients with degenerative spinal stenosis. Depending on the etiology, epidural lipomatosis may resolve after reduction or cessation of the causative factor, such as cessation of steroid therapy, bilateral adrenalectomy, or weight reduction. Multilevel laminectomy with debulking of the epidural fat produces neurological improvement in more than 75% of cases. |
Revised
11/22/06
Copyrighted 2006. David C Preston