|
A 45 year-old woman presented for evaluation of poorly controlled temporal lobe seizures, despite taking three anticonvulsant medications. Her seizures always started with a "deja vu" feeling, followed by staring into space and picking at her clothes. |
![]()
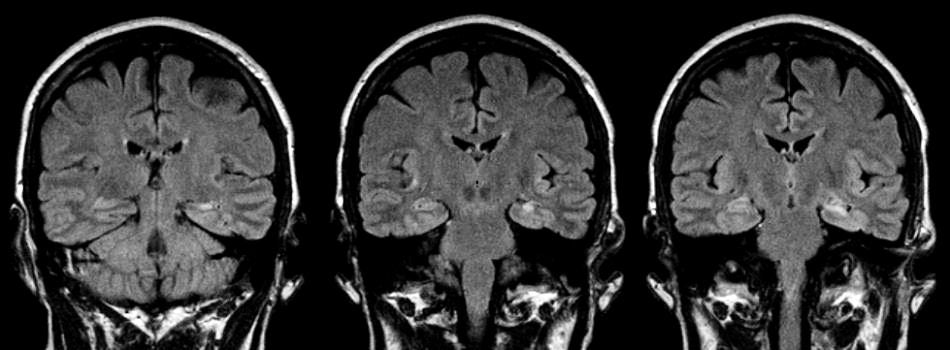
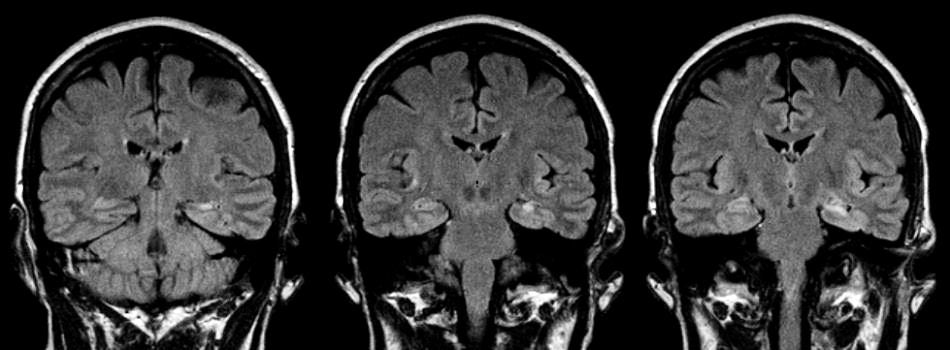
| Mesial Temporal Sclerosis:
Flair coronal MRIs. Note the bright signal in
the left hippocampus. This lesion was the source of the patient's
seizures. Subsequent EEG recordings showed a persistent left
temporal focus.
Temporal-lobe epilepsy is the most common type of epilepsy in adults. In most, the seizure focus originates in the mesial temporal lobe (hippocampus, amygdala, and parahippocampal gyrus), resulting in complex partial seizures (CPS). The most common pathology in surgically resected specimens is that of mesial temporal sclerosis (gliosis and scarring in the mesial temporal lobe). The etiology of mesial temporal sclerosis is controversial. It is thought to possibly result from an early injury to the brain or congenital malformation. It is an important diagnosis to recognize as these patients can often be made seizure free with surgical resection of the mesial temporal lobe. CPSs often begin with an aura followed by decreased responsiveness, a motionless stare, and decreased awareness of oneself and the environment (altered consciousness, not loss of consciousness). The aura is often emotional, olfactory or gustatory (i.e., an odd feeling, or unpleasant smell or taste). During a CPS, the patient appears awake. There is no loss of muscle tone, convulsions, tongue biting or urinary incontinence. Hence, CPSs may be difficult to recognize, especially for the non-neurologist. One of the important clues to a CPS is the presence of automatisms (involuntary, coordinated movements or behavior that occur during a state of clouded consciousness) that may occur in the course of a CPS. Patients may continue their ongoing motor activity or react to their surroundings in a semipurposeful manner. Verbal automatisms range from simple vocalizations, such as moaning, to more complex stereotyped speech. Motor automatisms are classified as simple or complex. Simple motor automatisms include oral automatisms (e.g., lip smacking, chewing, swallowing) and manual automatisms (e.g., picking, fumbling, patting). Complex motor automatisms consist of elaborate, coordinated movements that involve the bilateral extremities (e.g., cycling movements of the legs and stereotyped swimming movements). |
Revised
11/04/06
Copyrighted 2006. David C Preston