|
A 54 year-old woman developed the sudden onset of difficulty seeing on the left side. In the ER, her EKG showed new onset atrial fibrillation. |
![]()
![]()
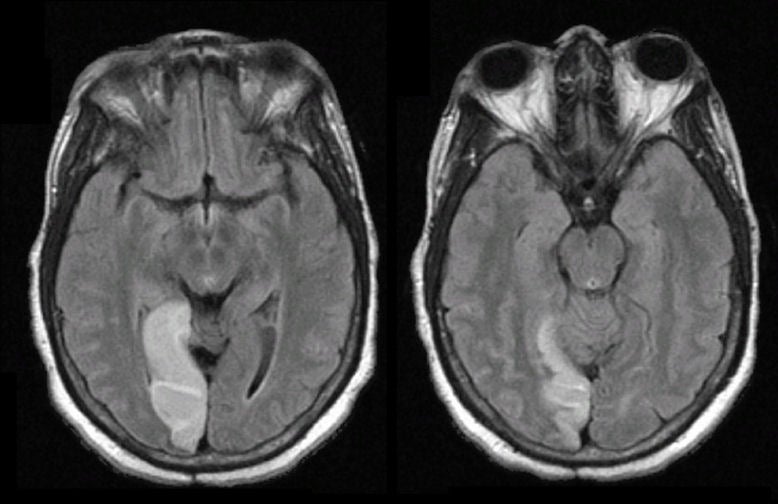
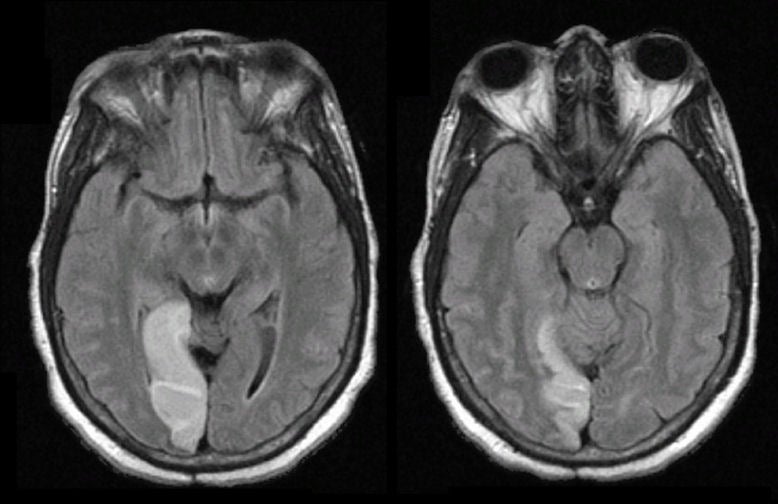
| Posterior Cerebral Artery (PCA) Infarction: Flair axial
MRIs. Note the bright signal in the right medial occipital lobe, in the
distribution of the right posterior cerebral artery. In this case,
the infarct was most likely caused by a cardiac embolus from the new
onset atrial
fibrillation. The basilar artery bifurcates into two PCAs at its termination, which then course around the midbrain in the ambient and quadrigeminal cisterns to supply the medial / inferior temporal lobe and the medial occipital lobe. Small perforators arise from the proximal PCAs, which supply the cerebral peduncle as well as the thalamus (the latter known as thalamoperforators). Infarctions in the territory of the PCA most often result in a contralateral hemianopsia. Other signs and symptoms depend on whether the infarction involves the thalamoperforator territory, and whether the infarction is left vs. right sided. Proximal PCA involvement results in coexistent infarction of the lateral thalamus, with contralateral hemisensory findings. Infarction of either PCA may result in impaired memory (verbal on the left; spatial on the right). In addition, left PCA lesions are sometimes associated with alexia without agraphia (patients can write, but cannot read what they have written); transcortical sensory aphasia (a receptive aphasia similar to Wernicke's aphasia except that repetition is relatively spared); and Gerstmann's syndrome (a combination of acalculia, finger agnosia, agraphia, and right/left confusion). With right sided PCA lesions, patients may have a visual neglect. They may also have prosopagnosia, an inability to recognize familiar faces. |
Revised11/23/06
Copyrighted 2006. David C Preston