|
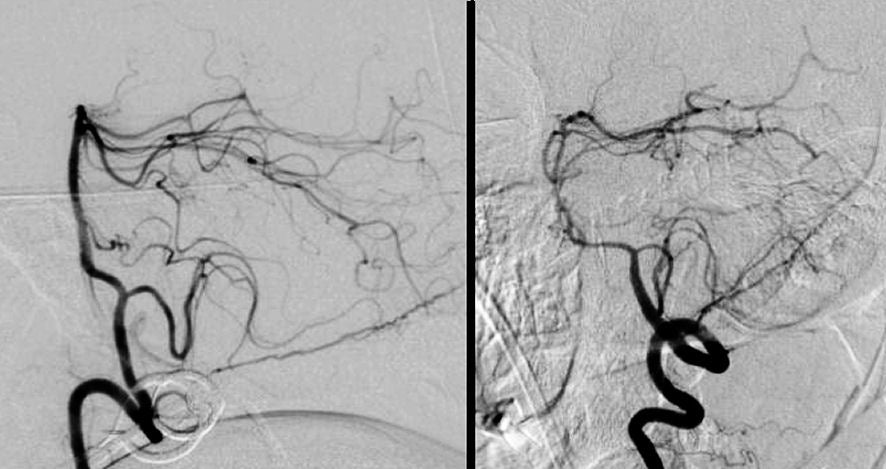
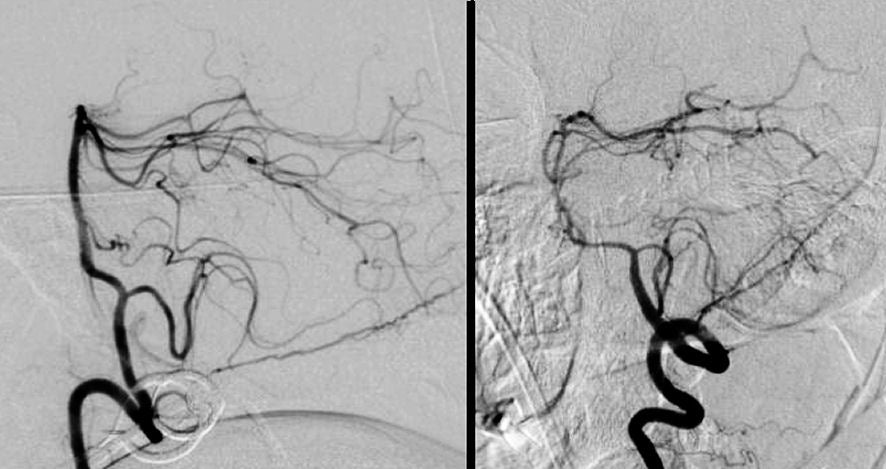
A 32 year-old woman developed the abrupt onset of a severe headache followed by a brief loss of consciousness. CT scan showed diffuse subarachnoid hemorrhage. On hospital day 7, she developed lethargy, slurred speech and diplopia. |
![]()
| Vasospasm following Subarachnoid Hemorrhage. Cerebral
angiogram, Left vertebral artery injection, Lateral view. (Left) Hospital day
1; (Right) Hospital day 7. Note the severe narrowing of the
basilar artery and its branches on hospital day 7 (right image). This is
the picture of vasospasm, a known delayed complication of subarachnoid hemorrhage (SAH). PICA = posterior inferior cerebellar
artery, SCA = superior cerebellar artery, AICA = anterior
inferior cerebellar artery, PCA = posterior cerebral artery. Vasospasm is reported to occur in as many as 70% of patients with SAH and is clinically symptomatic in as many as 30% of patients. It most commonly occurs 4-14 days after the onset of bleeding. If severe enough, vasospasm may lead to progressive ischemia and stroke. In some cases, the acute stroke then results in edema, herniation and death. Vasospasm is typically treated with the calcium channel blocker nimodipine, volume expansion, mild elevation of blood pressure, and in some cases, angioplasty of the involved blood vessels. All of these treatments are better tolerated after the aneurysm has been successfully treated. |
Revised
11/21/06.
Copyrighted 2006. David C Preston