|
A 49 year-old woman developed the abrupt onset of loss of vision in her right visual field. |
![]()
![]()
![]()
![]()
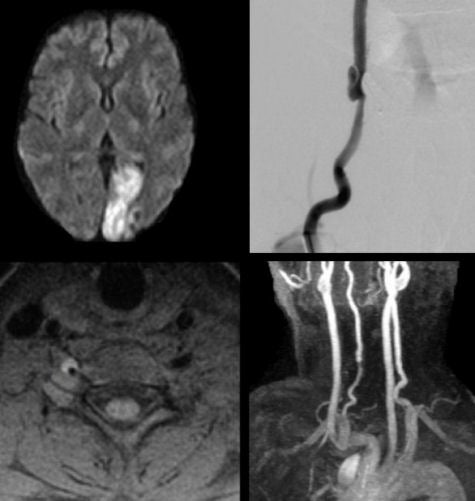
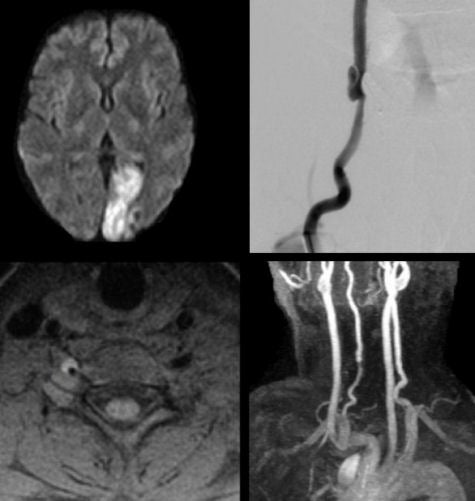
| Vertebral Artery Dissection: (Top Left) Diffusion-weighted
axial MRI. Note the acute infarct in the distribution of the left posterior cerebral
artery. (Top Right) Cerebral angiogram of the right vertebral artery. Note the
narrowing followed by outpouching in the right vertebral artery. This is
one of the angiographic appearances of a dissection. As blood dissects into the
wall and narrows the lumen, a smooth tapering of the vessel is seen; as blood
dissects and expands the wall, a pseudo-aneurysm develops - both are seen here. (Bottom Left) Fat suppression axial MRI.
Note the bright crescent shaped lesion
surrounding the right vertebral artery. This is blood in the wall of the vessel.
(Bottom Right) Gadolinium-bolus MRA of the aortic arch and major
cerebral vessels. Note the narrowing of the mid-lower right vertebral artery. If the diagnosis of dissection is suspected, fat-suppression MRI is the imaging study of choice. Intramural blood can be well demonstrated on these scans. Routine magnetic resonance angiography (MRA) will often demonstrate narrowing or occlusion of the vessel, but in most cases cannot differentiate dissection from other etiologies. It is critical to detect a dissection before ischemia occurs, so that treatment can be promptly initiated. Arterial dissection occurs due to a tear in the intimal layer of the artery. The tear allows blood to enter the wall and form an intramural hematoma. Depending on which layer of the blood vessel is involved, either a subintimal or a subadventitial hematoma develops. A subintimal hematoma tends to cause stenosis of the artery, whereas a subadventitial hematoma often results in aneurysmal dilatation of the artery. In the case of stenosis, sluggish blood flow distal to the dissection results in the formation of fibrin clot. The clot continues to enlarge and eventually breaks off to travel and dislodge downstream as an embolus. Although rare in the general population, dissections of the carotid and vertebral arteries account for a substantial number of strokes in young adults and middle-aged patients. Most dissections involve some type of trauma or stretch to the head or neck. Sometimes, the trauma is trivial and forgotten by the patient. There is a higher incidence in certain congenital connective tissue disorders, including Marfan's syndrome, cystic medial necrosis, and fibromuscular dysplasia. The recognition of an arterial dissection requires a high degree of clinical suspicion and an ability to recognize some key neurological signs which help to key in on the diagnosis. The classic symptoms and signs of vertebral artery dissection
include the following: • Pain in the back of the neck,
although it can be diffuse or frontal |
Revised
11/07/06
Copyrighted 2006. David C Preston