![]()
![]()
![]()
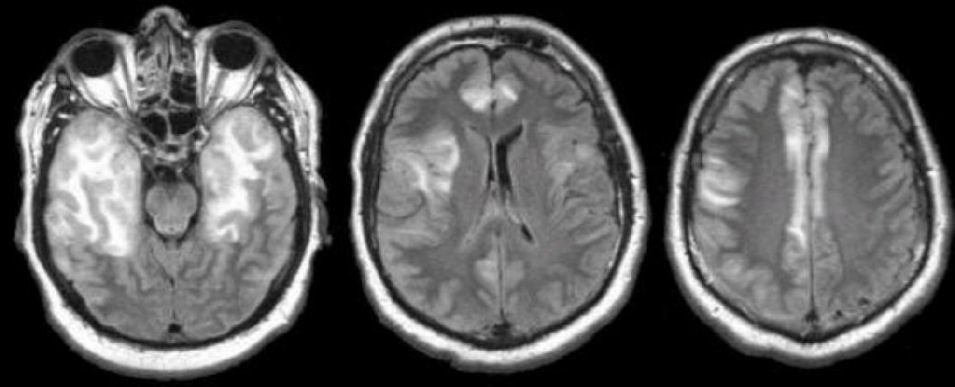
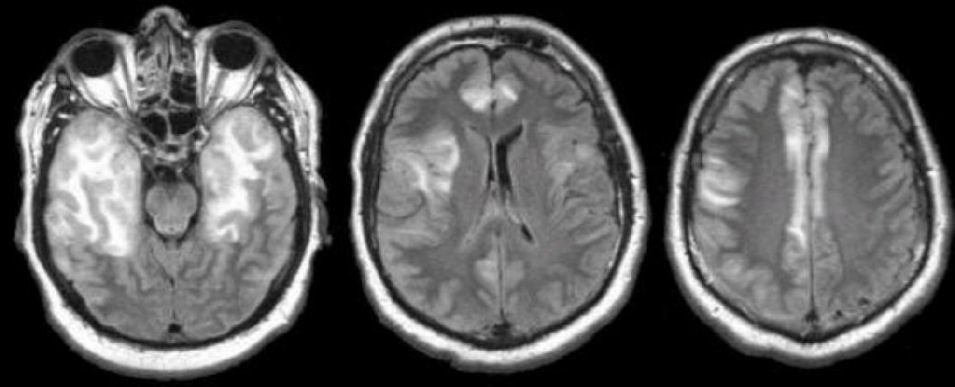
| Herpes Simplex Encephalitis:
Flair axial MRIs. Note the abnormal (bright) signal in both temporal lobes
(left image). Also note the involvement of the insula on the right side (middle
image) and the
cingulate gyrus bilaterally (middle and right images). CSF PCR subsequently confirmed the diagnosis of Herpes encephalitis. Herpes simplex virus (HSV) is a double stranded DNA virus which typically affects neonates or adults. Infection occurs either through hematogenous spread (most common route in the neonatal period) or retrograde neuronal spread (adult). Two strains of herpes simplex virus, HSV-1 and HSV-2, are the responsible pathogens for herpes simplex encephalitis (HSE), the most common non-epidemic encephalitis. HSV-2 results in genital lesions, and accounts for almost 90% of neonatal and almost all congenital infections. HSV-1 is exceedingly common, typically causing oral lesions (i.e., fever blisters), and is most commonly associated with HSE in adult patients (95%). HSE occurs from retrograde neuronal spread of latent virus from a previously infected ganglion into the brain, causing a hemorrhagic and necrotizing meningoencephalitis. The current thinking is that primary or recurrent herpes infection (usually HSV-1) ascends to the temporal lobe via trigeminal or olfactory tracts. Adult-onset HSE typically localizes to the temporal and frontal lobes; in neonates the encephalitis is characteristically more diffuse. Severe edema, petechial hemorrhage, and massive hemorrhagic tissue necrosis can be seen on gross specimens. The characteristic feature of HSE is hemorrhagic necrosis of the temporal lobe. Infection tends to begin unilaterally, only spreading to the contralateral temporal lobe in the late stages of disease. HSE has no gender or racial predilection. Its incidence has a bi-modal distribution, peaking in childhood and middle-aged adults. It comprises about ten percent of all encephalitis cases, occurring in 1 in 150,000 Americans, and is the most common cause of sporadic fatal encephalitis. The presentation can vary from aseptic meningitis to rapidly progressive encephalitis. Presenting symptoms include headache, fever, meningeal signs and altered consciousness. As the temporal lobes are often affected, other symptoms are common, including language dysfunction (mainly receptive aphasia due to lesions of Wernicke’s area), memory loss, and behavioral changes. Patients often experience focal seizures. HSE is a neurological emergency. Left untreated, it is rapidly progressive and often fatal. If one suspects HSE, one should initiate the work up rapidly and start treatment immediately. Imaging studies include CT and MRI. MRI with gadolinium is the preferred study. Bilateral medial temporal and inferior frontal regions are usually affected. Localized temporal abnormalities are highly suggestive of HSE. CT scan may show temporal or frontal changes, but almost a third of patients with HSE have a normal CT scan. However, the lesions may not be apparent for 3-4 days after presentation. Electroencephalography (EEG) is very sensitive and is abnormal in 80% of patients with HSE. Typical findings include diffuse slowing, focal temporal changes, periodic complexes, and periodic lateralizing epileptiform discharges (PLEDS). These latter findings are highly suggestive of HSE, in the proper clinical context. While EEG is highly sensitive, it lacks specificity. Once a space occupying lesion is ruled out via head CT, lumbar puncture should always be performed. CSF analysis typically shows a mononuclear pleocytosis with an elevated or normal protein, and normal to reduced glucose. Because HSE is often hemorrhagic, RBCs are typically elevated in the CSF, as evidenced in all collected tubes. CSF studies should include HSV-1 and HSV-2 PCR for DNA. PCR is highly sensitive and specific and has replaced brain biopsy as the standard for diagnosis. PCR is reported as 98% sensitive, and remains positive for 5 days following initiation of anti-viral treatment. Viral culture is rarely positive. Serum viral antibody titers become positive after 10 days to 2 weeks. Intravenous acyclovir is the drug of choice. It should be initiated once the diagnosis is suspected in order to reduce mortality, shorten the clinical course, and prevent complications. Acyclovir reduces mortality by 50% (from 60-70% to 30%). The mortality rate in untreated individuals nears 70%, and 20% among treated patients. Moreover, 50% of survivors have moderate to severe permanent neurological deficits. More than half of HSE survivors endure long-term neurological sequelae. Anterograde memory is often impaired even with successful treatment. Retrograde memory, executive function, and language function may also be impaired. Prognosis is directly related to time until treatment; those treated earliest after presentation tend to have a better prognosis. |
Revised
11/30/06
Copyrighted 2006. David C Preston