|
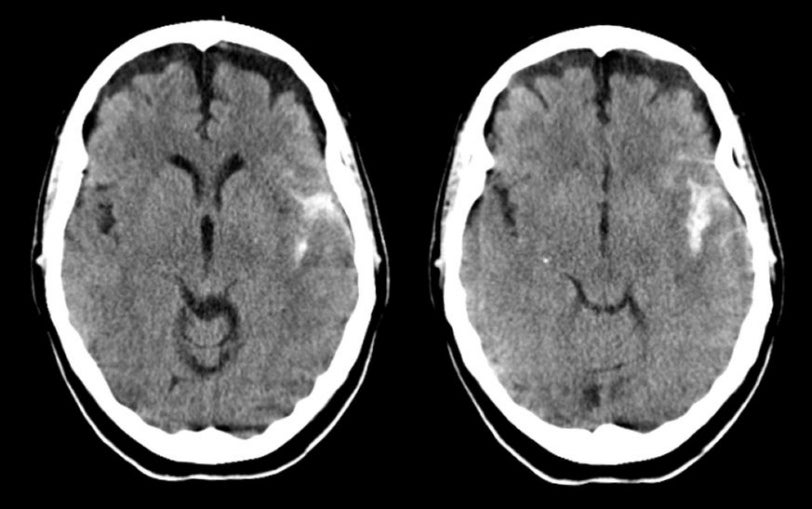
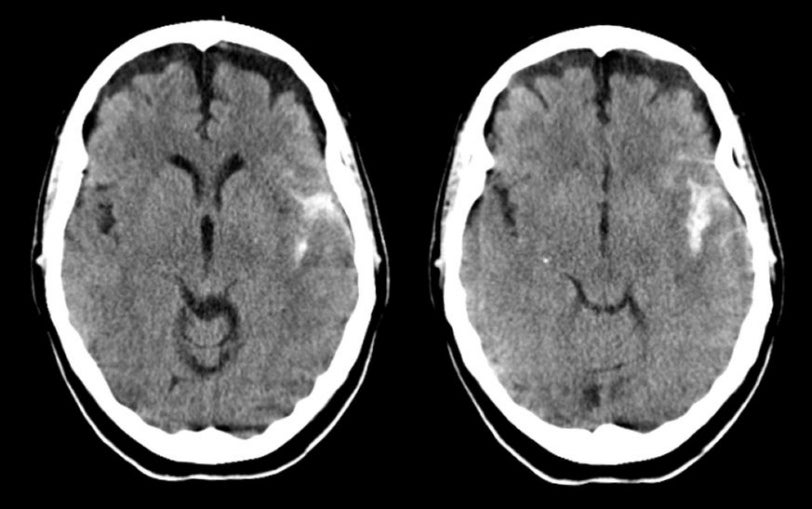
A 44 year-old woman developed the abrupt onset of an explosive headache. On exam, she was obtunded with right sided weakness. |
![]()
![]()
| Subarachnoid Hemorrhage - Middle Cerebral Artery Aneurysm.
Axial CT scans without contrast. Note the blood in the left Sylvian fissure. In some
instances of subarachnoid hemorrhage, the area with the most blood will suggest the
correct location of the aneurysm. In this case, the bleeding was
from a left middle cerebral artery aneurysm. Also note the prominent
frontal subdural fluid collections bilaterally. These fluid collections
are most likely subdural hygromas. Hygromas are subdural collections of
cerebrospinal fluid (CSF), without blood. The collection typically
results from a traumatic tear in the arachnoid, with a subsequent
leak of the CSF into the subdural space. On CT scan, it may be very
difficult to differentiate a hygroma from a chronic subdural
hematoma. MRI can easily make this determination as remote blood on
MRI is associated with a specific pattern on T1- and T2-weighted
images. Subarachnoid hemorrhage (SAH) is the extravasation of blood into the subarachnoid space between the pial and arachnoid membranes. The most common causes of spontaneous SAH are rupture of a saccular (berry) aneurysm (80%) and rupture of an arteriovenous malformation (AVM) (10%). Aneurysm formation is also seen in the setting of mycotic aneurysms, as well as in association with some congenital disorders, including coarctation of the aorta, Marfan's syndrome, Ehlers-Danlos syndrome, fibromuscular dysplasia, and polycystic kidney disease. Causes of non-aneurysmal SAH include amyloid angiopathy, blood dyscrasias, fibromuscular dysplasia, Moyamoya disease, and vasculitis (10%). Aneurysms are usually located in the intracranial arteries which lack an external elastic lamina and have a very thin adventitia. They lie unsupported in the subarachnoid space. The early precursors of aneurysms are small outpouchings through defects in the media of the arteries. These defects expand as a result of hydrostatic pressure from pulsatile blood flow and blood turbulence. The probability of rupture is related to the tension on the aneurysm wall. From the Law of La Place, the tension on the wall is proportional to the diameter. Thus, the rate of rupture is directly related to the size of the aneurysm.. Aneurysms usually occur at arterial bifurcations and mostly arise from the anterior circulation of the Circle of Willis (85%). The most common sites of aneurysms include: Posterior communicating artery Sentinel, or "warning" leaks that produce minor blood leakage are reported to occur in 30-50% of cases. Sentinel bleeds produce sudden focal or generalized head pain that may be severe. They also result in nausea, vomiting, photophobia, malaise, or, less commonly, neck pain. Sentinel bleeds precede aneurysm rupture by a few hours to a few months, with a reported mean of two weeks prior to discovery of the SAH. Aneurysms can present with a variety of symptoms and signs, the following being the most common: A sudden onset of severe headache
("thunderclap headache"), often described as the worst headache of
my life" |
Revised
11/22/06.
Copyrighted 2006. David C Preston