|
An 82 year-old man fell out bed. Afterwards, he became confused and unsteady in his walking. |
![]()
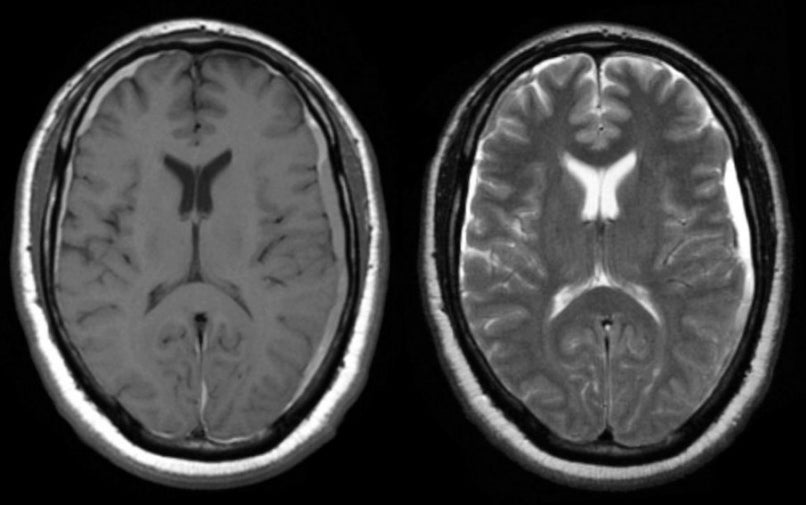
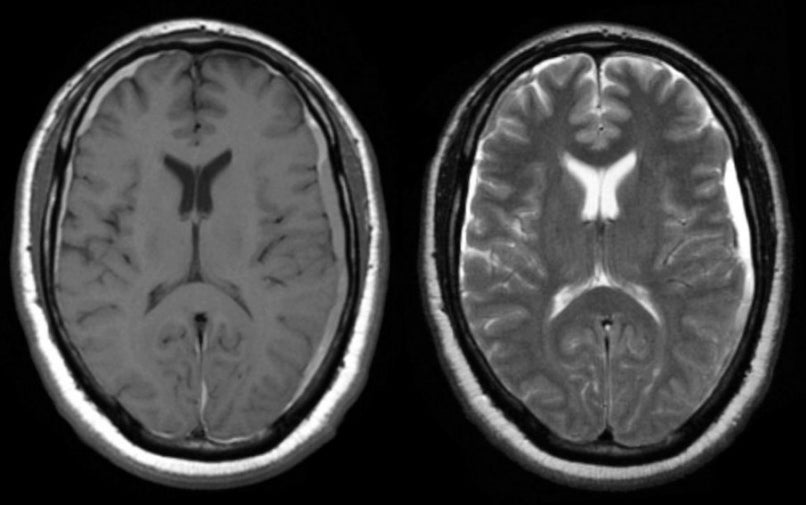
| Bilateral Subdural Hematomas (Acute). (Left) T1-weighted
axial MRI; (Right) T2-weighted axial MRI. If one looks closely, one
sees the thin crescent shape overlying and compressing
the left hemisphere. The signal is bright on T2- and dark on T1-weighted
images, signifying acute blood . Also, note
there is a small subdural hematoma in the contralateral frontal lobe, seen best on
the T1-weighted image. Subdural hematomas are recognized by their crescent shape overlying and compressing the brain. They are arbitrarily divided into three types: acute (< 4 days), subacute (4-21 days) and chronic (> 21 days). In the acute stage, blood is bright on CT. Eventually in the chronic state, the blood turns dark. In the subacute stage, a variety of patterns can be seen. Most common is layering of the plasma over the blood cells, creating a picture similar to spun whole blood. During this stage, the subdural hematoma may be isointense, making it difficult to see on CT, especially if it is small. The findings of blood on MRI are more complex and depend on timing. To learn more, review the powerpoint slide show, Blood on MRI: Time-dependent Changes. Acute subdural hematomas are the most common type of intracranial traumatic lesion. They are especially common in the elderly, in whom they may occur following insignificant and often forgotten head trauma. This is one the most common etiologies because as the brain atrophies, which is more common in the elderly, the "bridging veins" that connect the cortex to the draining venous sinuses stretch, and are more easily torn from minor trauma, resulting in a subdural hematoma. Clinically, subdural hematomas may present in a variety of ways. Most often, there is some cognitive change with subtle contralateral neurological findings (e.g., a mild hemiparesis). This is in contrast to intraparenchymal lesions (i.e., ischemic or hemorrhagic stroke) wherein the contralateral neurological findings (e.g., weakness, sensory loss, visual field abnormalities) are often quite prominent. As a subdural hematoma expands, it deforms the underlying brain, illustrating the Monro-Kellie Doctrine, which states that in an adult the cranial volume is a constant. The cranial contents consist primarily of brain, cerebrospinal fluid (CSF) and blood vessels. If the patient develops an expanding subdural hematoma, these elements must shift to accommodate the mass. Since the cranial volume is a constant, part of the cranial contents will herniate through the tentorial incisura to make room for the mass. The mortality rates of an acute subdural hematoma are as high as 90%. |
Revised 11/29/06.
Revised
11/29/06.
Copyrighted 2006. David C Preston