|
A 35 year-old man with multiple sclerosis had a history of 1-2 attacks every year. |
![]()
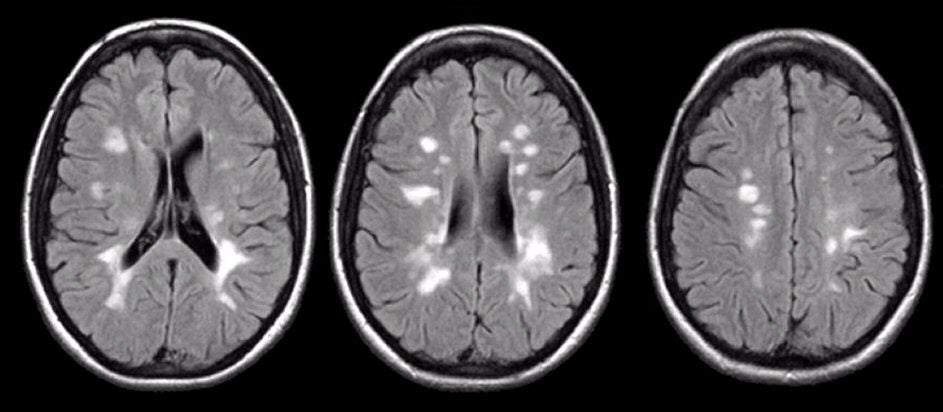
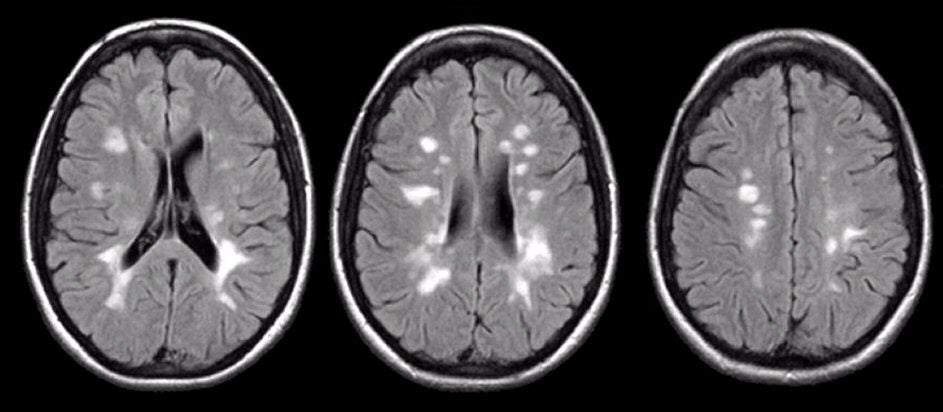
| Multiple Sclerosis (MS): Flair axial MRIs. Note the
numerous demyelinating lesions in multiple areas of the white
matter. Most of the lesions are near the ventricles. Several are
aligned perpendicular to the ventricles, a pattern which is often
seen in multiple sclerosis, and commonly referred to as "Dawson's
fingers". Over time, the demyelinating lesions may become
confluent. MS is a common neurological disorder, and one of the leading causes of disability in young adults. It is characterized by recurrent neurological episodes separated by time and space, resulting in multiple demyelinating lesions in the central nervous system. Because MS affects different areas of the brain, brainstem, cerebellum and spinal cord, a variety of neurological symptoms and signs can be seen. The most common temporal course in MS is a relapsing/remitting pattern. Patients with this temporal course experience intermittent neurological attacks that last days to weeks. Patients often recover to their baseline, whereas others may have some residual deficit following an attack. A minority of patients have a chronic progressive course. Many patients with a relapsing/remitting course will evolve into a chronic progressive course years into their disease. Similar to many other autoimmune disorders, MS is more common in women than in men. MS most commonly presents in young adults, although any age can be affected. MS affects the myelin in the CNS, with relative preservation of the axons. The etiology is unknown, but many observations point to an autoimmune pathogenesis. MS plaques usually develop in a perivenular distribution, and are characteristically seen in the periventricular white matter, brainstem, and spinal cord. The active lesions contain T lymphocytes and macrophages. A variety of neurological symptoms and signs are seen in patients with MS. These may include cognitive, visual, cranial nerve, corticospinal, sensory, cerebellar, bladder and/or sexual impairment. Certain clinical syndromes are highly suggestive of MS, especially in the appropriate age group. These include: • Optic neuritis - Optic neuritis presents as an acute unilateral loss of vision (mainly central vision), often accompanied by pain in the eye, that worsens with eye movement. On examination, an afferent pupillary defect is usually present. • Internuclear Ophthalmoplegia (INO) - This characteristic horizontal eye movement abnormality results from a lesion in the medial longitudinal fasciculus (MLF) which runs through the pons and midbrain. In a patient with an INO, when the patient looks to one side, the abducting eye moves correctly, but the adducting eye is restricted. Often, the abducting eye movement is accompanied by nystagmus. However, with a convergence maneuver, both eyes move correctly, denoting that the medial rectus and cranial nerve III are intact. Unilateral and bilateral INOs are most commonly seen in patients with MS. In a younger patient, the presence of an INO is almost always due to MS. In older individuals, an INO can be see in a brainstem stroke (typically due to basilar ischemia). • Uhthoff's phenomenon - This refers to a worsening of neurological symptoms with an increase in body temperature (e.g., following exercise, a hot bath, or fever). This phenomenon occurs because transmission through demyelinated segments of nerve fails at higher temperatures. • Lhermitte's phenomenon - Lhermitte's phenomenon
refers to a
transient "electric shock" or "buzzing" sensation that runs down the
spine or into the limbs when the neck in flexed (note: this sign can
also be seen in structural lesions compressing the spinal
cord, e.g., spondylosis, tumor, etc.). Diagnostic Evaluation of a Patient with Suspected MS Until the advent of MRI, MS was often difficult to diagnose with certainty. Brain CT is unable to visualize the demyelinating plaques, and thus usually normal in a patient with MS. In the past, the diagnosis was based on a clinical course of a relapsing and remitting neurological disease (two or more deficits separated in time and space) in the appropriate age group, and in the absence of another explanation. The diagnosis was often supported by: • CSF Abnormalities - The protein is often elevated with a mild lymphocytosis. In addition, signs of myelin breakdown and an ongoing immune response may be seen, especially during an attack (e.g., elevated myelin basic protein, the presence of oligoclonal bands, elevated IgG synthesis rate). • Demonstration of "Silent" Lesions - Evoked potentials (EPs) were often used to confirm the presence of additional subclinical lesions. These tests are done by stimulating an afferent pathway (visual, auditory or sensory) and recording their resultant potentials over the brain using scalp electrodes, similar to those used during EEG. Visual evoked potentials are useful in detecting subclinical lesions of the optic nerves and visual pathways; auditory evoked potentials are able to detect lesions in the brainstem (thus, they are also known as brainstem evoked potentials); and somatosensory evoked potentials assess the posterior columns and rostral sensory pathways. Although CSF studies and EPs were often used in patients with suspected MS, many times the results were normal or equivocal. In addition, these studies are not specific to MS; thus, false positives can occur. • Magnetic Resonance Imaging - MRI has markedly improved the ability to diagnose MS correctly. Not only is MRI able to exclude conditions that may mimic MS clinically, but it is also able to show the characteristic demyelinating plaques in over 90% of patients. These plaques are typically located in the deep white matter, especially in a periventricular pattern. They are also seen in the brainstem, cerebellum and spinal cord. Management and Treatment of MS The treatment of MS involves both symptomatic and disease modifying therapy. Symptomatic therapy is available for spasticity, tremor, fatigue, bladder dysfunction, depression, and cognitive impairment. Intravenous methylprednisolone (Solu-Medrol) is used during acute attacks to promote a quicker recovery. It is most commonly used in optic neuritis. It is also used for any attack wherein the symptoms are serious enough to interfere with daily functioning. However, this treatment likely does not change the natural history of the disease. Several disease-modifying drugs are now approved by the FDA in patients with relapsing/remitting MS. These include: • Interferon ß-1b (Betaseron) • Interferon ß-1a (Avonex and Rebif) • Glatiramer acetate/copolymer 1 (Copaxone) Each of these agents have been shown to significantly reduce the relapse rate and the burden of lesions on MRI. Each is given as an injection, either by a subcutaneous or intramuscular route. They vary in how often they are given: once a week for Avonex, three times a week for Rebif, and daily for Betaseron and Copaxone. As a general rule, all patients with relapsing forms of MS should receive one of these agents indefinitely. Treatment of the chronic progressive form of MS is more problematic. A variety of immunosuppressive regimens have been tried, including total lymphoid radiation, methotrexate, cyclophosphamide, mitoxantrone, and azathioprine. Each of these are nonspecific immunosuppressive agents. While they may halt a rapidly progressive course, they are problematic when used indefinitely as they can be associated with significant toxicity and risks. The risk-benefit ratio must be assessed on a case by case basis. |
Revised
11/29/06
Copyrighted 2006. David C Preston