features
A Bold Quest
Anirban Sen Gupta and research colleagues on campus and around the country are on a mission to create a lifesaving blood substitute
 Photo by Roger Mastroianni Anirban Sen Gupta
Photo by Roger Mastroianni Anirban Sen GuptaBLOOD MEANS LIFE.
It means family. It seals a promise. It boils, curdles and rushes, runs icy and hot, signifies weakness and strength. Spilled, it can mean death.
But to Anirban Sen Gupta, PhD, blood is something else: It’s a challenge. For close to two decades, Sen Gupta—a Case Western Reserve University biomedical engineering professor—has been developing artificial blood platelets and therapeutics to manage bleeding.
Now, he is leading a campus team, working with researchers at multiple universities and biotechnology companies on an even more ambitious quest: to create a lab-made substitute for whole blood. The Defense Advanced Research Projects Agency (DARPA) at the U.S. Department of Defense is backing the project with a four-year, $46.4 million grant.
If Sen Gupta and his colleagues succeed, their work could be lifesaving.
Every year more than 60,000 people in the United States—and more than 2 million globally—die from bleeding complications, Sen Gupta said. And millions more receive blood transfusions, including people with cancer or sickle cell disease, patients losing blood during surgery or in labor and delivery, and victims of car accidents and gunshot wounds. According to a 2020 study cited in a federal report to Congress, transfusions are among the most frequent procedures performed in U.S. hospitals.
But the whole enterprise teeters on one fragile, needle-thin pillar: donated blood, which is constantly in short supply. There is no other source, Sen Gupta said.
Unless, of course, it can be manufactured.
"Nature has created this intricate life-force of a fluid over millions of years of evolution," said Sen Gupta, the Wallace R. Persons Endowed Professor of Engineering, "and trying to emulate that synthetically is a very complex and audacious venture."
THE PROMISE OF PLATELETS
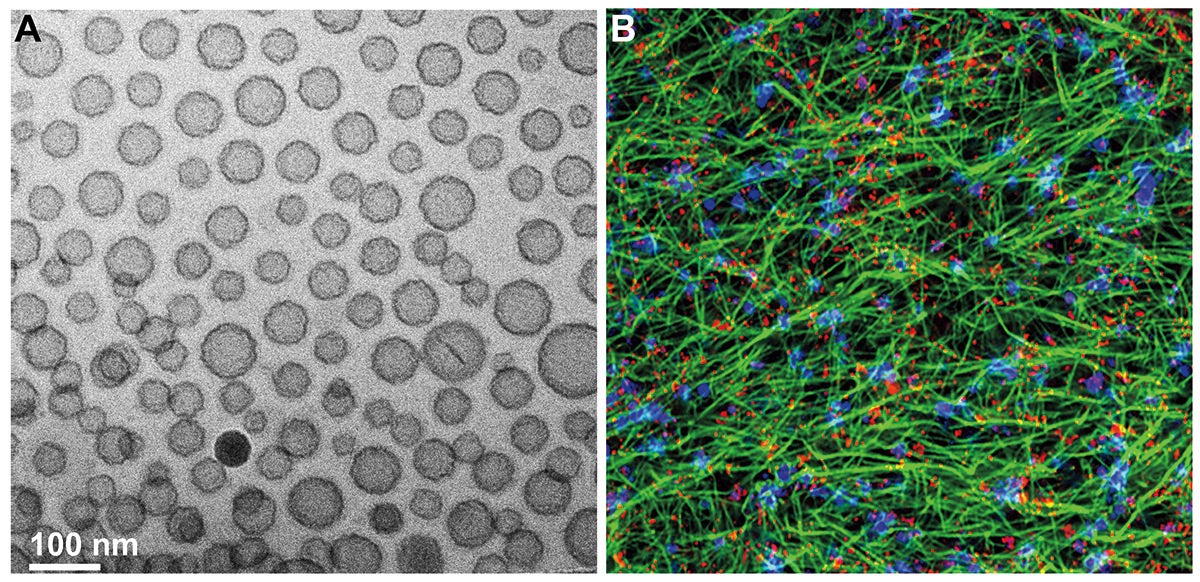 IMAGE CREDIT A: Sen Gupta Lab and Haima Therapeutics;
IMAGE CREDIT A: Sen Gupta Lab and Haima Therapeutics;IMAGE CREDIT B: Sen Gupta LabAnirban Sen Gupta and his team have developed synthetic-platelet nanoparticles that help generate and stabilize clots to stop bleeding. On the left is an electron microscopy image of these synthetic platelet nanoparticles; on the right is a high-resolution fluorescence image of a blood clot, showing fibrin mesh (a protein formed in clots) in green, platelets in blue and nanoparticles in red.
Blood is not just one thing: It’s an entire ecosystem, a society, a universe. That’s one reason it is so difficult to replicate synthetically. It contains three main types of cells, each with a different function. Red blood cells carry oxygen. White blood cells fight infection. Platelets are indispensable in forming clots to stop bleeding from an injury. Plasma, the liquid part of blood, ferries all those blood cells, as well as water, proteins, hormones, salts and nutrients, wherever the body needs them. All these components must work in harmony in blood circulation.
Plasma can be freeze-dried and stored at room temperature for a year or more, but red blood cells, chilled, stay functional for only 42 days. Platelets only last up to seven days at room temperature and possibly three weeks if chilled, Sen Gupta said, making them the weakest link in the blood-transfusion chain.
Platelets are his specialty. The smallest of the blood cells, each tinier than a speck of powdered sugar, they function like a team of biological building inspectors, constantly scrutinizing the body for injury and bleeding. Once found, they jump to fix it, linking to frame a patch then plastered into place by a protein called fibrin. A platelet can respond to an injury within nanoseconds, with pinpoint accuracy to stop the bleed in a process called hemostasis.
Sen Gupta first took on the problem of synthetic platelets after joining CWRU’s biomedical engineering faculty in 2006. As he and his students studied the history of artificial blood, they recognized an opportunity: "We realized that all the past work on ‘artificial platelets’ focused only on a single mechanism of how platelets help form clots, whereas, in reality, you need multiple platelet mechanisms happening in tandem to effectively form a clot," Sen Gupta said.
His solution takes that multipronged approach. It involves taking lipid nanoparticles and "decorating" them with molecules that help them stick to the site of the injury and to each other, while signaling the body to dial up production of fibrin at the injury site.
In 2014, Sen Gupta and his former student, Christa Pawlowski, PhD (CWR ’11; GRS ’15, biomedical engineering), patented the lab’s artificial platelet technology. And in 2016, they co-founded the startup Haima Therapeutics, which licensed the technology from CWRU and named it SynthoPlate. The company has since received funding from the Department of Defense, the National Institutes of Health and the National Science Foundation to advance the technology toward clinical use. (Sen Gupta serves as Haima’s chief technology officer; Pawlowski the chief operating officer.)
Haima also developed a process for freeze drying SynthoPlate into a powder form to make it easier to store and transport. Sen Gupta envisions a future in which a cache of shelf-stable, freeze-dried artificial platelet powder is standard in ambulances and in medical kits carried on the battlefield or by civilian first-responders in response to mass-casualty events.
"Dried artificial blood products are the future of resuscitation medicine," said Philip Spinella, MD, a professor of surgery and critical care medicine at University of Pittsburgh and codirector of its Trauma and Transfusion Medicine Research Center. Spinella, who also serves as associate medical director at Pitt’s Center for Military Medicine Research, has collaborated with Sen Gupta for almost a decade. He values Sen Gupta’s dedication to bridging basic science with real-life clinical medicine: "Many scientists claim to be translational scientists," he said, "but Anirban is the real deal."
RECREATING WHOLE BLOOD
 Photo by Roger MastroianniAnirban Sen Gupta reviewing research with Shruti Raghunathan, an American Heart Association fellow and doctoral researcher in his lab.
Photo by Roger MastroianniAnirban Sen Gupta reviewing research with Shruti Raghunathan, an American Heart Association fellow and doctoral researcher in his lab.Sen Gupta’s work is the latest chapter in a pursuit that goes back hundreds of years. Beginning in the 1600s, physicians tried to cure disease and treat hemorrhage with various blood substitutes—lamb’s blood, calf’s blood, even milk— with little success. Those efforts were sidelined in the 20th century as a series of breakthroughs, many driven by battlefield medicine during the world wars, made human-to-human blood transfusions a practical reality. Though it’s impossible to say how many lives were saved by these advances, during World War I, only 4% of injured U.S. soldiers survived their wounds; in World War II, 50% did, according to a paper cited in a Department of Defense article.
But blood loss can still be deadly, especially for civilians and armed forces who cannot get to a medical facility in time. "In austere battlefield scenarios, more than 80% of deaths are from bleeding out," Sen Gupta said.
While Sen Gupta and his campus team are focused on artificial platelets, collaborators nationally are working in parallel on fully or partially synthetic versions of other blood components. Over years of meetings and conferences, they have speculated about what it might take to combine their products and create a substitute for whole blood.
Their conversations ramped up in the early months of the COVID-19 pandemic, when blood donations were at a minimum, triggering a national blood-donation emergency. But they knew that such a monumental project would require a level of funding, intellectual property know-how and commercialization expertise beyond any one research lab’s capacity.
Enter DARPA and its project seeking solutions to hemorrhages in the field. Last year, the agency announced its planned $46.4 million investment in the project to create artificial whole blood. The project is led by the University of Maryland, Baltimore and includes an interdisciplinary team from CWRU, Haima Therapeutics, KaloCyte Inc., Teleflex Inc., University of Pittsburgh, The Ohio State University, University of California San Diego and several other partner organizations.
In addition to providing freeze-dried artificial platelets through Haima Therapeutics, Sen Gupta is leading the CWRU team that is performing lab tests to evaluate the safety and efficacy of the artificial whole blood.
The goal is to make a blood substitute that can be freeze-dried and kept at room temperature, a blood equivalent of the dehydrated, shelf-stable military rations called MRE. This "whole blood analogue" would be lightweight, portable and shelf-stable: just add water (or saline), warm it and go.
"We would actually be able to transport a usable product that could be mixed in the field and used in the moment, even in very isolated places," said Shannon E. French, PhD, the Inamori Professor in Ethics at CWRU. She is leading the project’s examination of the ethical, legal and social implications of the blood substitute.
"I’ve lost friends and colleagues in combat," said French, who also co-directs the university’s master’s degree program in military ethics. "To think that the work that’s being done here could possibly save lives like theirs in the future is very moving." The substitute could also help save tens of thousands of civilians in the United States and more than 2 million globally who die from hemorrhage.
"Many people die because they don’t have access to simple transfusions or blood products," said Umut Gurkan, PhD, the Wilbert J. Austin Professor of Engineering and professor of Mechanical and Aerospace Engineering at CWRU. He studies blood disorders in low- and middle-income countries and is part of the multi-institution research team.
The problem extends beyond supply. "Think of refrigeration," Sen Gupta said. "Think of distribution. Think of blood banking. Think of the logistics of how you get it from the donor to the patient."
In resource-limited settings—including rural communities in the United States, where patients may be hours away from the nearest hospital—a freeze-dried substitute would be transformative. "We could stockpile it for a long time and use it on demand as needed, so we don’t constantly have to look for donors, look for storage, look for transport," Sen Gupta said.
In addition to SynthoPlate, the whole blood analogue will include a red blood cell product called ErythroMer, being developed by overall project leader Allan Doctor, MD, professor of pediatrics at University of Maryland School of Medicine. The third ingredient is freeze-dried plasma from Teleflex, a medical technology company based in Pennsylvania.
The CWRU team is running lab tests on various formulations of the whole blood substitute. Harihara Baskaran, PhD, the Leonard Case Jr. Professor of Engineering and chair of the Department of Chemical and Biomolecular Engineering, is testing to see how the blood substitute flows through a lab model of blood vessels to observe the reaction to a material with properties different from human blood. Meanwhile, Gurkan is using tiny blood-vessel-simulating devices to see how the blood substitute behaves on endothelial cells, which line human blood vessel walls.
If the blood is cleared for safety in lab testing, the next phase will be testing its safety and efficacy in preclinical models of traumatic bleeding. If all goes well, it could be ready for clinical trials around 2028.
Meanwhile, Sen Gupta and his campus colleagues are continuing to advance synthetic platelets as a stand-alone clotting aid for emergencies like postpartum hemorrhage and complex surgeries. "Anirban is at the forefront of this mission," Spinella said, "and many of us are betting on him to get it done."
BLOOD BY THE NUMBERS
The average adult has five liters of blood. A newborn has about one cup.
The first recorded successful human-to-human blood transfusion was just four ounces, given to a woman experiencing postpartum hemorrhage around 1820. The donor was the patient’s husband.
The U.S. blood-banking system collects about 13.6 million units (one unit is about a pint) of donated blood annually.
Nearly 30,000 units of whole blood, 6,000 units of platelets and 6,000 units of plasma are transfused every day in the United States.
Only about 3% of the eligible population donates blood every year in the United States.
Sources: various academic studies, American Red Cross and America’s Blood Centers





