Increasing corporatization, private equity investment, and pressures on private practice are having a major effect on the organization of medical care and the experiences of patients and clinicians.
That was the message delivered by Lawrence Casalino, MD, PhD, to an audience of medical students, faculty, alumni, and community members at the inaugural Wisdom of Practice lecture on October 8, 2022. Dr. Casalino, an expert in public health and population health sciences at Weill Cornell College of Medicine, is a family physician, a sociologist, and a national figure in health care policy and research.
The lecture was followed by a panel discussion on health care corporatization with Dr. Casalino; Evelyn Duffy, DNP, RN, Florence Cellar Professor of Gerontological Nursing at the Frances Payne Bolton School of Nursing; and Scott Alperin, DDS, chief of Dentistry & Oral and Maxillofacial Surgery at Hillcrest Hospital.
The Wisdom of Practice initiative is supported by the University Suburban Health Center Foundation to investigate how health care brings value to the lives of the people it serves and the effect of contextual factors, such as practice ownership.
The Health Care Corporatization Trend
Corporatization is well-entrenched in American health care, according to Dr. Casalino. Large regional and national hospital systems and insurers (which increasingly own medical practices and employ clinicians) are expanding, and a growing number of health care entities are for-profit or have adopted for-profit behaviors. In addition, private equity and venture capital firms, which expect a quick return on investment, are increasing their acquisition of medical and dental practices.
The trend toward corporatization was exacerbated by the pandemic, as smaller practices struggled to survive.
Among the facts and figures Dr. Casalino presented as evidence of the growth of corporatization:
- An estimated 60-65% of physicians are now employed by hospitals or corporate entities.
- The combined revenues of two publicly traded corporations (CVS/Aetna and UnitedHealth Group) = 14% of total US health spending
- UnitedHealth Group is larger than the British National Health Service and ExxonMobil.
Pros and Cons
While corporate ownership has a number of benefits—including, for employees, the possibility of greater work-life balance and career advancement, and, for large organizations, more investment in data systems to meet quality process measures (although the impact on overall quality is not known)—the trend to corporatization raises concerns:
- Consolidation of power: The larger health care entities become, the more they can influence and benefit from policy, allowing them to become even larger.
- Patient mix: Large health care organizations focus not only on serving patients and improving care; they also focus on increasing profits by attracting patients who are well-insured and relatively easy to care for.
- The future of professionalism: Compared to smaller and in-person practices, will physicians in corporate organizations and telehealth settings have,
- The same relationship with their patients?
- The same ability to personalize patient care?
- The same sense of commitment?
- Intrinsic motivation: If professionalism is compromised, what will it mean for patient care, clinician autonomy, and the ability of practices to "go the extra mile” for patients?
Glimpsing a Different Future
While the shift to corporatization is significant, it is not the only factor shaping the health care landscape.
In another Wisdom of Practice event, medical students learned about Direct Primary Care, an innovative practice and payment model gaining traction in the US. DPC is characterized by an affordable membership fee, without fee-for-service payments or third-party billing, a high level of patient access to their physician, and the opportunity for a strong patient-clinician relationship.
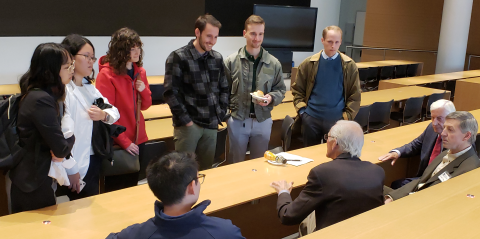
The rise of relationship-focused practice models, such as DPC, offers both a contrast to corporatization and a path for change. In an animated informal conversation following the two events, medical students and Wisdom of Practice advisory board members discussed the promise of emerging practice models to balance health care's status quo by prioritizing relationships, community involvement, and decision-making by those providing care.


![Photo of Larry Casalino standing on stage next to a podium and in front of a large screen projecting a slide titled Organizational Size [and] Policy Feedback Loop](/medicine/healthintegration/sites/default/files/styles/article_300x300_/public/2023-01/Casalino%20lecture4.png?h=079dc941&itok=R1c_uBn4)