The brain MRI is important for the diagnosis of prion disease for ruling out other possible etiologies, but it can also show features suggestive of prion disease. Brain MRI findings are found in most contemporary criteria for the diagnosis of sporadic Creutzfeldt-Jakob disease (sCJD), including the Centers for Disease Control and Prevention's (CDC) criteria1.
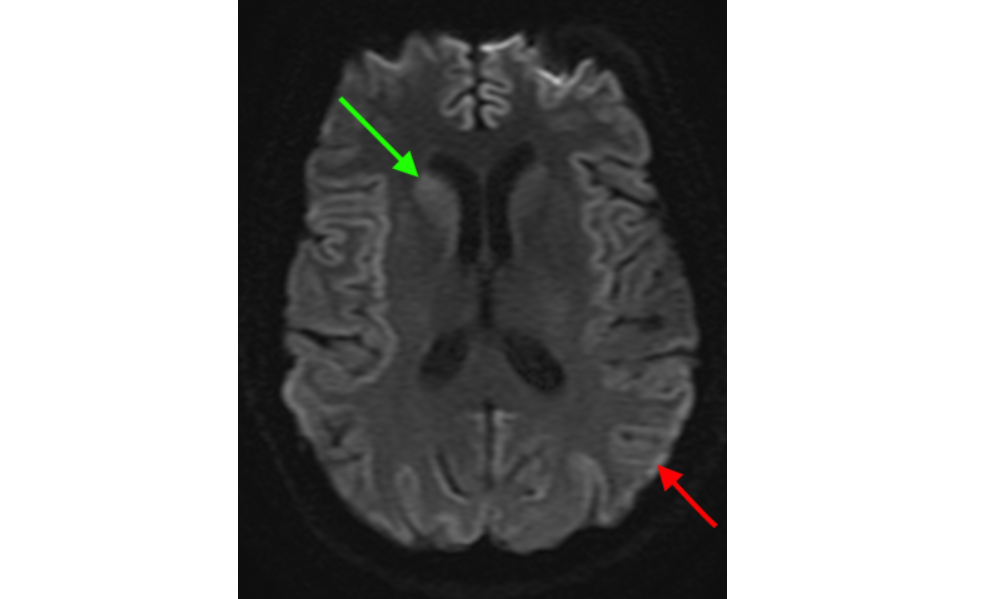
Brain MRI criteria include hypersensitivity on diffusion-weighted imaging (DWI) or fluid-attenuated inversion recover (FLAIR), with DWI being the most sensitive MRI sequence. A brain MRI suggestive of sCJD demonstrates hyperintensity in the caudate and putamen, and/or at least two cortical regions (temporal, parietal, occipital), the latter of which is often referred to as "cortical ribboning" (Figure)2. Sensitivity and specificity using these diagnostic criteria vary between 69-76% and 90-100% respectively, depending on the reader3.
Other brain MRI diagnostic criteria propose a suggestive MRI as defined by one positive brain region (frontal, parietal, temporal, and occipital lobes, caudate, putamen, and/or thalamus) on DWI3. This new criterion increases diagnostic sensitivity to 90-95% with little change to specificity. Restricted diffusion, as demonstrated on apparent diffusion coefficient (ADC) mapping, is helpful in differentiating prion diseases from other etiologies that may mimic similar brain MRI findings4. Brain MRI changes usually begin early in the disease process and may be the first thing to raise clinical suspicion of prion disease5.
The aforementioned MRI findings are most likely due to spongiform changes occurring in the brain6. Because neuropathologic characteristics differ among the different types of prion disease, brain MRI patterns likewise differ depending on sCJD molecular subtype7. Similarly, although some cases of genetic prion disease may demonstrate a suggestive brain MRI, some mutations may not. Variant Creutzfeldt-Jakob disease (vCJD), a unique prion disease usually caused by eating meat contaminated with bovine spongiform encephalopathy (BSE), is marked by hyperintensity in the thalami, especially in the pulvinar nucleus (pulvinar of "hockey stick" sign), primarily on FLAIR sequences8.
The NPDPSC has an MRI Consultation Program that will offer the clinician a free-of-charge reading of the MRI as it pertains to the likelihood of prion disease. Reports can only be sent to physicians; therefore, this individual's contact information, including an appropriate fax number or email address, should accompany the scan.
If you are interested in submitting Brain-Only MRI Images to our center for MRI consultation, please read the guidelines and fill out the "MRI Interpretation Request Form", both located on this page.
Turnaround time for MRI consults is 3-4 business days.
References
1. Centers for Disease Control and Prevention. Diagnostic Criteria: CDC’s Diagnostic Criteria for Creutzfeldt-Jakob Disease (CJD), 2018. https://www.cdc.gov/prions/cjd/diagnostic-criteria.html
2. Zerr I, Kallenberg K, Summers DM, Romero C, Taratuto A, Heinemann U, et al. Updated clinical diagnostic criteria for sporadic Creutzfeldt Jakob disease. Brain 2009;132:2659–68. https://doi.org/10.1093/brain/awp191.
3. Bizzi A, Pascuzzo R, Blevins JE, Grisoli M, Lodi R, Moscatelli M, et al. New criterion for detecting prion disease with diffusion magnetic resonance imaging: Diagnostic performance and comparison with cerebrospinal fluid tests in a large autopsy cohort. JAMA Neurology 2020;132:2659–68.
4. Vitali P, Maccagnano E, Caverzasi E, Henry RG, Haman A, Torres-Chae C, et al. Diffusion-weighted MRI hyperintensity patterns differentiate CJD from other rapid dementias. Neurology 2011;76:1711–9. https://doi.org/10.1212/WNL.0b013e31821a4439.
5. Satoh K, Nakaoke R, Nishiura Y, Tsujino A, Motomura M, Yoshimura T, et al. Early detection of sporadic CJD by diffusion-weighted MRI before the onset of symptoms. J Neurol Neurosurg Psychiatr 2011;82:942–3. https://doi.org/10.1136/jnnp.2008.155242.
6. Manners DN, Parchi P, Tonon C, Capellari S, Strammiello R, Testa C, et al. Pathologic correlates of diffusion MRI changes in Creutzfeldt-Jakob disease. Neurology 2009;72:1425–31. https://doi.org/10.1212/WNL.0b013e3181a18846.
7. Meissner B, Kallenberg K, Sanchez-Juan P, Collie D, Summers DM, Almonti S, et al. MRI lesion profiles in sporadic Creutzfeldt-Jakob disease. Neurology 2009;72:1994–2001. https://doi.org/10.1212/WNL.0b013e3181a96e5d.
8. Zeidler M, Sellar RJ, Collie DA, Knight R, Stewart G, Macleod MA, et al. The pulvinar sign on magnetic resonance imaging in variant Creutzfeldt-Jakob disease. The Lancet 2000;355:1412–8