Neurocritical Care Boot Camp Prepares Future Advanced Care Practitioners
Story by Helen Jones-Toms
Photographs by Roger Mastroianni
Amid the antiseptic stillness of the cadaver lab is a quiet hum of conversation. Students and instructors huddle around two tables: one with a male patient and one with a female. Only the tops of their heads are visible from beneath their drapes.
After receiving instructions from Ben Roitberg, MD and fellow neurosurgeon Robert Geertman, MD, PhD, FAANS, a first-year MSN student prepares to drill burr holes. It’s the first part of the procedure to measure cranial pressure. The student is noticeably timid. Roitberg reminds her that she can’t hurt the patient.
Still, it’s not easy to take a hand drill to someone’s skull, living or dead.
“Hold the drill this way—perpendicular to the skull,” prompts Roitberg, chair of Neurosciences and Neurological Surgery at MetroHealth Medical Center. “Gentle pressure. Let the drill do the work. You will feel a slight tug when you hit the inner layer of the skull—the composition of the bone changes.”
The student listens intently as she continues her work. Once completed, she breathes a sign of relief, removes the drill, gently twists the screw into the bone and dresses the wound.
Welcome to boot camp.
HIGH DEMAND FOR THE HIGHLY SKILLED
Neurocritical Care Boot Camp, jointly sponsored by the Frances Payne Bolton School of Nursing at Case Western Reserve University and MetroHealth Medical Center, is a two-day continuing education seminar to prepare advanced practice providers to practice in the field of neurocritical care. It’s the brain child of Chris Winkelman, PhD, ACNP, FAANP, FCCM, associate professor at FPB and Molly McNett, PhD, RN, CNRN, director of nursing research at MetroHealth, and adjunct FPB faculty.
Winkelman says, “I have seen the volume of Adult-Gerontology Acute Care Nurse Practitioner students and employment opportunities grow substantially in the eight years since I’ve been lead faculty for this track at FPB. I’ve recently seen up to ten open positions for Neuro APRNs— advanced practice registered nurses or nurse practitioners— across the major hospitals in Northeast Ohio, alone.”
“We felt the Neurocritical Care Boot Camp provided a great way to bridge education, science, and practice,” Chris Winkelman, PhD, ACNP, FAANP, FCCM
“The majority of my research is in clinical neuroscience and neurocritical care,” McNett says. “Neurocritical care is a fast-growing subspecialty, highly reliant on skilled APRNs—yet there are no training programs to ensure advanced practice registered nurses (APRN) have the special skill set required to function effectively in this role.”
McNett adds, “I knew by partnering with ChrisWinkelman and Case Western Reserve, we could jointly meet that demand by pooling resources and collaboration.” Open to APRNs and physician assistants (PAs), the camp is designed for seasoned, new, and in-training advanced practice providers interested in a career working with patients who required neurocritical care. The interprofessional program includes didactic, simulation, and skills-based learning led by nurse practitioners, researchers, neurosurgeons and pharmacologists.
DAY ONE: CRANIAL CLASSROOM AND DURA DISCUSSIONS
On the mandatory first day of the seminar, 26 attendees focus on learning or re-learning anatomy and physiology, neurocritical care management, neuropharmacology, neuroimaging, and best practice guidelines. Lectures held on the Case Western Reserve campus were followed by exercises to engage learners and apply content.
For example, following the neuroradiology lecture, participants moved from Mondo board to Mondo board—oversized touch screens with internet connectivity. They reviewed X-rays, magnetic resonance images (MRIs), computerized tomography (CT) scans, and other tests as if in a mock Grand Rounds. Each station had expert-led discussion to hone diagnostic reasoning. In another exercise, pharmacologic approaches to treatment were detailed in small groups.
“In the course of the day you see students gain confidence in prescribing and in reading and interpreting images when we went on ‘image rounds,’” says Winkelman.
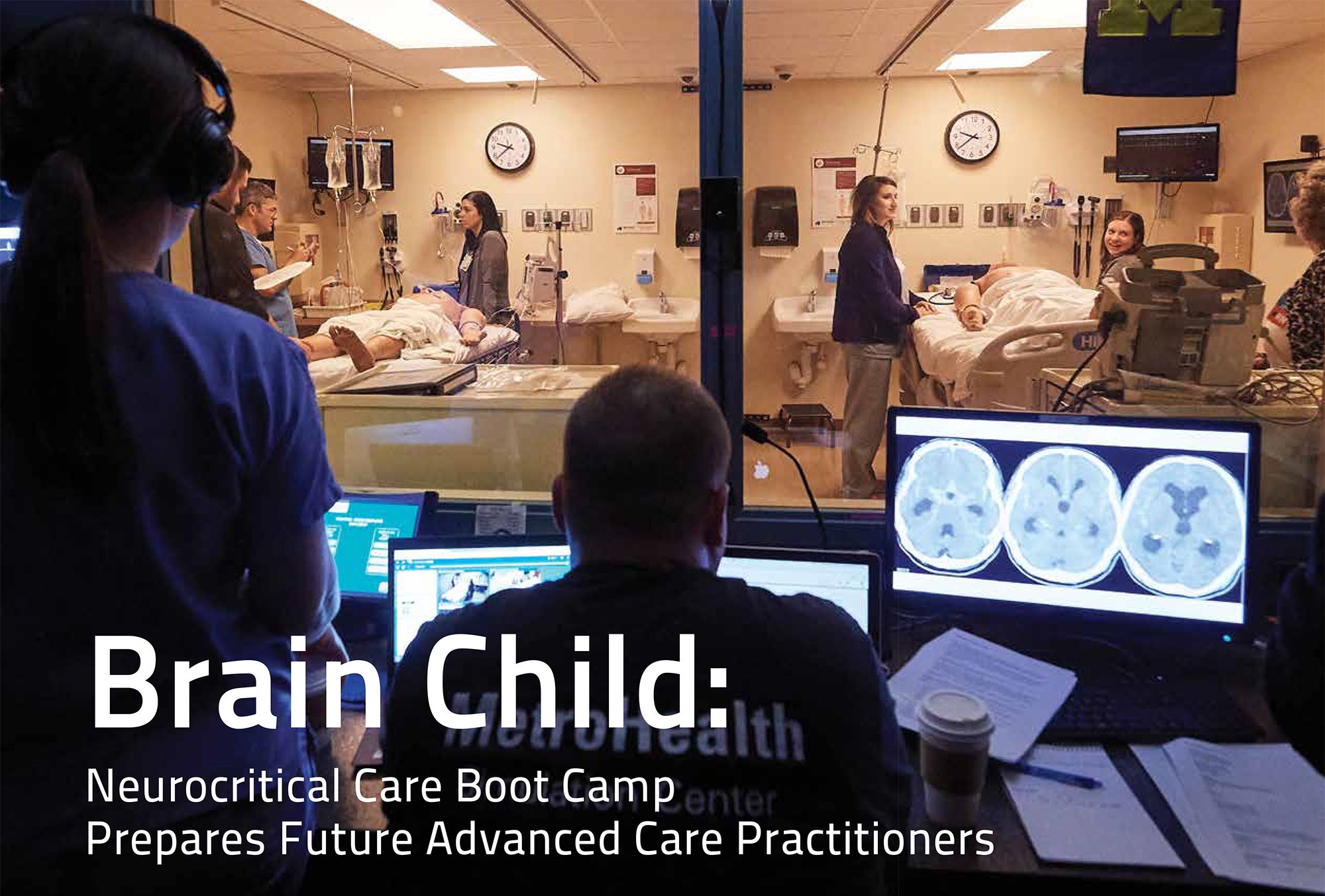
Twelve participants attend the optional second day, which provides on-site training at the MetroHealth Simulation Center on complex patient management. They practice placement of invasive lines and monitoring devices, suturing, and communicating with interdisciplinary teams. The emphasis is on realistic, hands-on training.
“Over the two days, you could see the participants gain insights into clinical decisions, along with ongoing resilience in an environment where uncertainty in outcome can be distressing,” Molly McNett, PhD, RN, CNRN
DAY TWO: ALL HANDS-ON TO SAVE THE BRAIN
Down the hall from the cadaver lab, another patient—a high-fidelity “Sim-Man”— is critically ill. In a simulated intensive care unit, the manikin lays on the bed with deteriorating neurological status and life-threatening changes in vital signs. The monitors alarm the unit “staff” who look to the boot camp participant to determine next steps. Behind the twoway mirror, the MetroHealth Simulation Center staff record the entire procedure as they manipulate monitor and Sim-Man remotely.
The patient’s “spouse”—played by Winkelman—walks in and sees the patient with wires protruding from his skull. She’s told that overnight the patient experienced brain swelling and the health care team had to intubate and place a device to monitor the pressure in the skull.
Wife Winkelman appears anxious. She leans over the patient and wistfully asks, “Can he hear me?”
Suddenly, the patient crashes as monitors beep violently. Winkelman ups her game as the hysterical spouse and cries, “What’s happening? What’s happening? Is he dying?”
The would-be staff member must now manage not only a critically ill patient but a frantic family member. She attempts to calm the spouse and usher her out of the room while picking up the phone to ask for the team to come help. Winkelman breaks character during the simulation.
“There is no team to call,” she states. “You ARE the team. You decide what to do next.”
The startled new member of the neuro acute care unit points at the professor and exclaims, “Right!” She starts checking vitals, assigning tasks, and asking for medications.
Once the exercise is complete, Winkelman returns to her Neuro Boot Camp faculty role and reviews the tape with the participants: what went well, went needs improvement and a review of the goals for learning are discussed. The atmosphere lightens. The newest graduates of the patient simulation station take selfies with faculty to capture their learning experiences as their video rolls in the background.
“I love working with patients who have neurological illness that requires acute and critical care,” says Winkelman. “It’s challenging and rewarding to work in an environment where human outcomes are uncertain and families drive so many decisions around care. I want to share the challenges of neurocritical care in a safe environment like Boot Camp and help others explore the field and be more confidant in that environment.”
“Over the two days, you could see the participants gain insights into clinical decisions, along with ongoing resilience in an environment where uncertainty in outcome can be distressing,” says McNett. “Plus, there is a renewed commitment to both best practices and familycentered care.”
Winkelman adds, “We felt the Neurocritical Care Boot Camp provided a great way to bridge education, science, and practice.”