August 2016
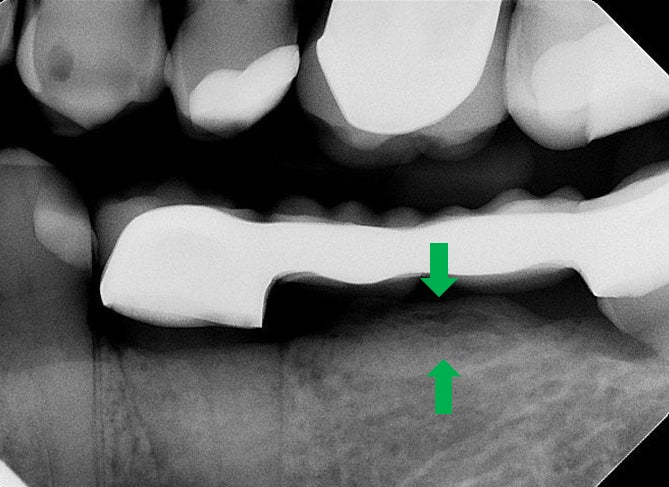
A 65-year-old male complains of food impaction in the lower left mandibular region. Clinical examination reveals a fixed partial denture. Bitewing radiographs show an increased density of the bone under the pontic (green arrows). Identify the abnormality and provide your diagnosis.
INCORRECT.
Mandibular tori are located on the lingual aspect; on radiographs they appear to superimpose over the roots of the premolar and molar teeth. However, in the bitewing radiographs shown, the radiopaque entity noted is below the pontic.
CORRECT.
There is a well-defined radiopaque entity noted at the crest of the edentulous alveolar ridge. Occasionally, irritation from the pontic could produce excessive bone formation, which would appear as a radiopaque entity under the pontic. Hence the entity noted in the bitewing is termed a subpontic hyperostosis.
August 2016 References
Koenig. Diagnostic Imaging: Oral and Maxillofacial. 1st Edition. Amirsys.
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
July 2016
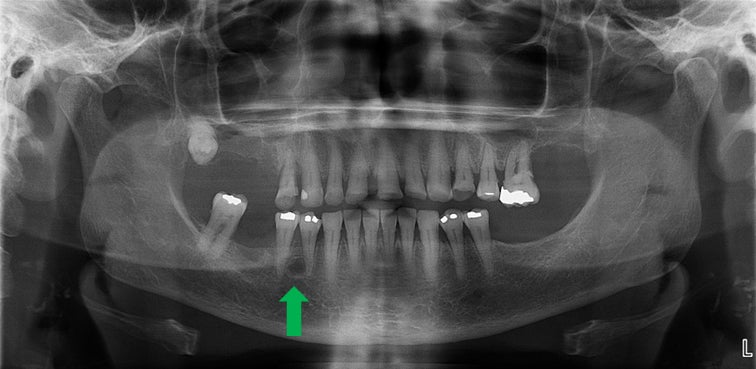
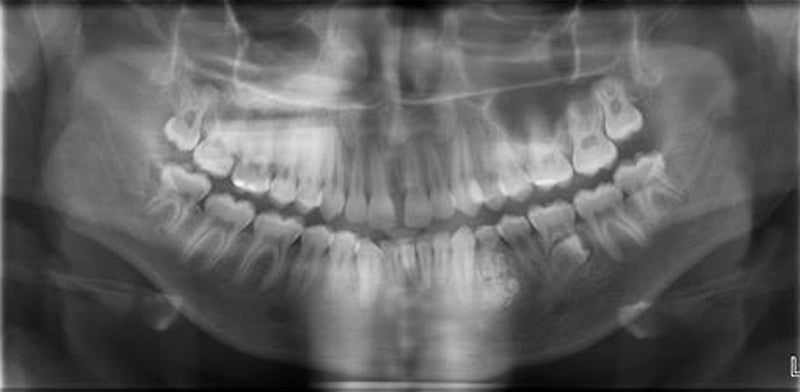
A 58-year-old female’s routine panoramic interpretation showed a well-defined radiolucency in the interradicular region (between #28 and 29). The lesion is well corticated, round to ovoid in shape. No evidence of root resorption or expansion is noted. Clinical examination proved that teeth are vital. Identify the abnormality and provide your diagnosis.
INCORRECT.
They are usually asymptomatic and are usually noted as an incidental finding. The radiographic appearance shows relatively smaller number of trabeculae in the cancellous bone. Periodic radiographic follow-up should shows no change.
CORRECT.
Based on the location and radiographic presentation, this fits the description of lateral periodontal cyst. The clinical exam should reveal vital teeth. Lateral periodontal cysts typically are noted in mandible, canine- premolar region. They are more prevalent in 5th or 6th decade. Lateral periodontal cyst if they are multiple they are termed as botryoid type.
INCORRECT.
Radiographically there is no evidence of loss of lamina dura and PDL space. Both lamina dura and PDL appears to be WNL. Coronally, no evidence of pulpal involvement is observed on the radiographs. Clinical examination should reveal teeth to be nonvital.
July 2016 References
Koenig. Diagnostic Imaging: Oral and Maxillofacial. 1st Edition. Amirsys.
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
June 2016
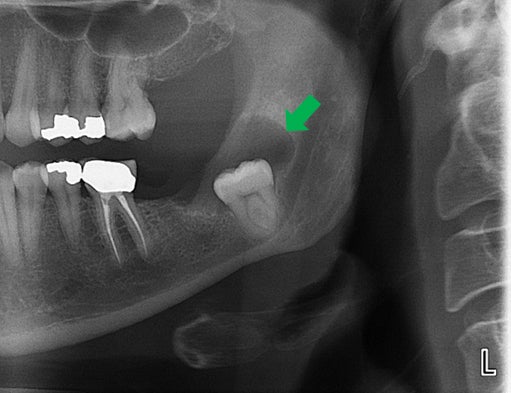
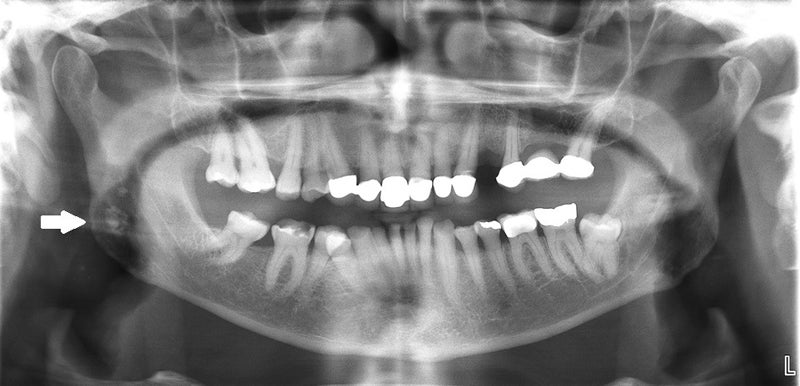
A 40-year-old female was referred by an oral surgeon to obtain a panoramic radiograph. Her chief complaint is mild discomfort in the lower left region. A cropped panoramic is displayed. A moderately well-defined radiolucency associated with an impacted tooth #17 (green arrow) is noted. What abnormality is depicted on this panoramic image?
INCORRECT.
Ameloblastic fibromas are benign mixed tumors. Generally they tend to occur at relatively younger age (average 15 years). Based on the age it can be ruled out.
INCORRECT.
Normal follicular space is in between 2-3 mm. If the follicular space is more than 3 mm and less than 5 mm one should consider hyperplastic follicle. Based on the radiographic presentation, it doesn’t fit the profile.
CORRECT.
The involved tooth demonstrates more than 5 mm of the follicular space, which is suggestive of a dentigerous cyst. One more key characteristic feature to observe on the radiograph is the epicenter of the lesion, located superior to the impacted tooth. The extent of the lesion appears to extend from CEJ to CEJ.
June 2016 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
May 2016
A 54-year-old female presented to the Oral and Maxillofacial Medicine and Diagnostic Sciences clinic with a chief complaint of, “I have cavities”. As a part of providing comprehensive care to the patient and to investigate the periapical region, radiographs were obtained. The upper anterior region showed a well-defined radiopaque entity (green arrow). Name the abnormality noted.
CORRECT.
Supernumerary teeth are supplemental teeth or additional teeth that are noted in the oral cavity. The morphology of the supernumerary tooth is generally altered. The size of the tooth will be miniature. Based on the location, the supernumerary are classified as a mesiodens (between central incisors), peridens (between premolars) and, distodens (between molars). Since the miniature tooth is located between central and lateral, the preferred term is supernumerary tooth.
INCORRECT.
A mesiodens is a supernumerary tooth that develops between two maxillary central incisors.
May 2016 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
April 2016
A 19-year-old female presents to the Oral Medicine and Diagnostic Clinic for a routine dental exam. After thorough clinical examination, radiographs are obtained and the right molar region periapical shows target-like presentation on the distal root of the #31 (green arrow). There is an intact PDL space surrounding the roots of the teeth. What is the likely diagnosis?
INCORRECT.
Hypercementosis is defined by an excessive deposition of cementum on the roots of the teeth, and presents without any clinical signs or symptoms. Radiographically hypercementosis demonstrates an excessive buildup of cementum on all or parts of the roots of the teeth. Most notably, the lamina dura and PDL space continue to encompass the expanded tooth.
INCORRECT.
Benign cementoblastoma is characterized by formation of slow growing cementum or cementum like tissue tissue attached to the apex of the tooth. On radiographs it is seen as a well-defined radiopacity with a cortical border and a radiolucent band inside the tumor. The apex of the affected tooth is often resorbed. Based on this radiograph, there is no evidence of root resorption.
INCORRECT.
Dense Bone Islands present asymptomatically and are most often found in the mandible of the premolar region. The periphery of the lesion is often well-defined but may also blend in to the trabeculae of the surrounding bone. There is no radiolucent border to these lesions.
CORRECT.
Severe curvature of the root is termed as dilaceration. The most common type of dilacerations occurs either mesially or distally. However, occasionally if the dilaceration of the root happens to occur either in the buccal or lingual direction, then the deflection from the root could give an appearance of bull’s eye (the apical foramen presenting as an eye and surrounding PDL space as radiolucent halo) from the central x-ray beam.
INCORRECT.
Periapical osseous dysplasia initially presents as a radiolucent lesion at the apex of the tooth. In later stages, the later lesion becomes radiopaque. This mature lesion is surrounded by thick sclerotic border with a retained radiolucent periphery. These lesions are most often found in the lower anterior region of the mouth.
April 2016 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
March 2016
A 19-year-old female presented to the Oral Medicine and Diagnostic Clinic. Radiographs were obtained and the panoramic radiograph showed a well-defined, round, radiopaque supernumerary tooth distal to the third molar. What is the likely diagnosis?
INCORRECT.
A mesiodens is a supernumerary tooth that develops between the maxillary central incisors.
CORRECT.
Supernumerary teeth are supplemental teeth, which may or may not be morphologically normal, that develop in addition to the normal set of teeth. They are result of excess dental lamina in development. Those that occur in the molar region are called distodens.
INCORRECT.
A peridens is a supernumerary tooth that develops in the premolar region.
March 2016 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
February 2016
A 63-year-old male presented to the Oral Medicine and Diagnostic Clinic. Radiographs were obtained and the pan showed generalized enlarged roots that were well-defined and radiopaque. There is an intact PDL space surrounding the roots of the teeth. What is the likely diagnosis?
INCORRECT.
Dense Bone Islands present asymptomatically and are most often found in the mandible of the premolar region. The periphery of the lesion is often well defined but may also blend in to the trabeculae of the surrounding bone. There is no radiolucent boarder to these lesions.
CORRECT.
Hypercementosis is defined by an excessive deposition of cementum on the roots of the teeth, and presents without any clinical signs or symptoms. Radiographically hypercementosis demonstrates an excessive buildup of cementum on all or parts of the roots of the teeth. Most notably, the lamina dura and PDL space continue to encompass the expanded tooth.
INCORRECT.
Benign cementoblastoma is characterized by formation of slow growing cementum or cementum like tissue tissue attached to the apex of the tooth. On radiograph it is seen as well-defined radiopaque with cortical border and radiolucent band inside the tumor. The apex of the affected tooth is often resorbed. Based on this radiograph, there is no evidence of root resorption.
INCORRECT.
Periapical osseous dysplasia initially presents as a radio lucent lesion at the apex of the tooth. In later stages, the later lesion becomes radiopaque. This mature lesion is surrounded by thick sclerotic boarder with a retained radiolucent periphery. These lesions are most often found in the lower anterior region of the mouth.
February 2016 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
January 2016
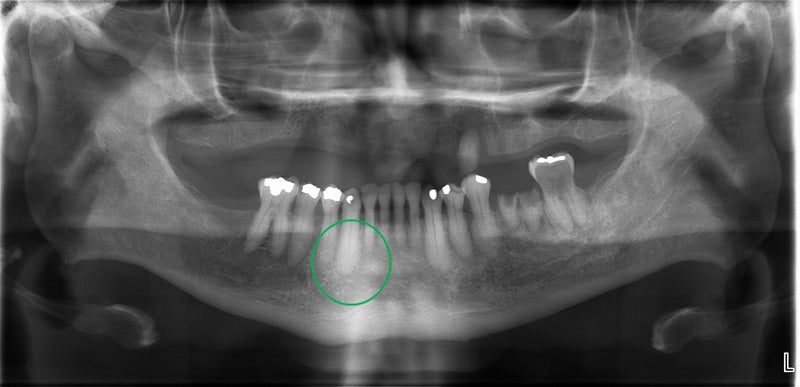
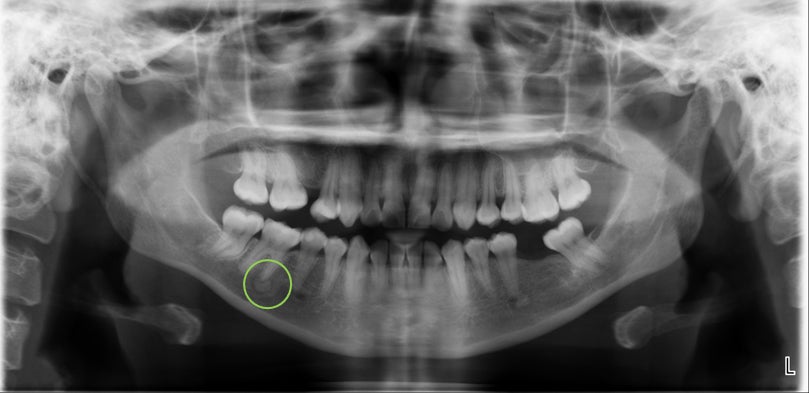
A 40-year-old African American woman was referred to evaluate the radiopaque entity surrounded by radiolucent structure centered over the apex of tooth #30 (circle). Upon vitality testing, both teeth were vital and no history of pain or sensitivity.
INCORRECT.
Benign cementoblastoma is characterized by formation of slow growing cementum or cementum like tissue tissue attached to the apex of the tooth. On radiograph it is seen as well defined radiopaque with cortical border and radiolucent band inside the tumor. The apex of the affected tooth is often resorbed. Based on this radiograph, there is no evidence of root resorption.
CORRECT.
Periapical osseous dysplasia is as result of reactive process where normal cancellous bone is replaced with fibrous tissue and cementum. It predominantly appears in mandibular anterior teeth. There are three different stages of the lesion: early stage radiolucent at the apex of the involved tooth with loss of lamina dura. Mixed stage radiopaque tissue surrounded by radiolucent structure. Mature stage, radiopaque structure with or without thin radiolucent margin at periphery. No treatment is indicated, but diagnosis is critical so it's not confused with other periapical disease.
INCORRECT.
Periapical rarefying osteitis is seen on the radiograph as a radiolucent lesion in the periapical area. The affected tooth should have a large carious lesion, spread into the apical region and the tooth is non-vital tooth. Based on the radiographic exam, there is no evidence of dental caries.
January 2016 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
December 2015
A 60-year-old woman presented to the Oral Medicine and Diagnostic Clinic. The panoramic revealed a cluster of small, ill-defined radiopacities found at the midportion of the right mandibular ramus (circle).
CORRECT.
Tonsilloliths are formed as a result of repeated bouts of inflammation. Incomplete resolution of organic debris such as bacteria and pus, epithelial cells can serve as a nidus for calcification. On a panoramic radiograph it appears on the mid ramus region as single or multiple cluster of radiopaque entities. Small calcifications usually produce no clinical signs or symptoms therefore no treatment is required. However, large calcifications with associated symptoms (such as halitosis) are removed surgically.
INCORRECT.
The most common location for calcified lymph nodes is submandibular region, near the angle of the mandible or between the posterior border of the ramus and cervical spine. Radiographically they are appear as a well-defined radiopacity with cauliflower-like shape. The location and shape is not consistent with calcified lymph nodes.
December 2015 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
November 2015
INCORRECT.
The shape and size are not consistent with root fragment. Additionally, there is no evidence of radiolucent pulp or radiopaque lamina dura surrounding the radiopaque entity.
CORRECT.
Antroliths are formed as a result of deposition of minerals. They are noted as incidental finding on the radiographs and are usually asymptomatic. On radiographs they appear as well defined, circumscribed radiopaque structures. The internal content is mostly homogenous and radiopaque in nature as noted in this panoramic radiograph. Large and symptomatic antroliths require referral to otolaryngologist for surgical intervention.
November 2015 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
October 2015
A 10-year-old female presented to the Pediatric Dental Clinic for her very first dental exam, radiographs, and prophy. On review of her pano, a radiopaque lesion at the apex of #20 extending coronal to approximately the mid-root was noted. Clinically, #20 had no carious lesions associated with it; no sign of fistula present, and no percussion sensitivity was noted.
INCORRECT.
Condensing osteitis is the sequelae of dental caries progressing into pulpal necrosis leading to increased radio density in the apical region of the tooth. Based on the radiographic exam there is no evidence of dental caries, lamina dura surrounding the tooth is intact and PDL appears to be WNL.
INCORRECT.
Periapical osseous dysplasia (POD) presents as a radiolucent entity in its initial phase, followed by radiopaque presentation in the mature stage. Mature stage is surrounded by thick sclerotic border. POD is most commonly seen in the lower anterior region.
CORRECT.
The region of interest demonstrates a solitary, well-defined, regular, smooth, radiopaque entity apical to #20 is noted. The internal aspect is uniformly radiopaque and there is no radiolucent rim surrounding this entity. It doesn’t appear to be causing any root resorption of #20. The localized area of revealing increased density that is not related to either inflammatory or dysplastic changes are referred as dense bone island or focal idiopathic osteosclerosis. Very rarely they can cause root resorption. No treatment is required for this condition.
October 2015 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
September 2015
A 41-year-old female presented to the oral medicine and diagnostic clinic with pain in the lower right mandible. After clinical examination, radiographs were obtained. The lower right PA showed two well-defined, radiopaque, lesions in relation to the root portion of tooth #30. The periphery appears to be smooth and continuous, producing a bulbous root portion. The likely diagnosis of this condition is?
INCORRECT.
The general presentation of cementoblastoma's growth is in a concentric fashion. Cementoblastoma are mixed density lesions with a radiating pattern, giving an appearance of a wheel spoke. Additionally, they can cause external root resorption. These characteristic features are missing.
CORRECT.
The internal architecture is more radiolucent than the tooth simulating cementum. The lamina dura and PDL are intact. The bulbous root portion is caused by excessive cementum, especially in the apical third of the root portion. The radiographic findings are consistent with hypercementosis.
INCORRECT.
Periapical apical sclerosing osteitis will be more diffuse with radiopaque sclerotic presentation and will not have a radiolucent rim.
September 2015 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
August 2015
A 37-year-old African American’s radiographs were referred for interpretation. No significant past medical history and non-contributory clinical findings were noted during clinical examination. Periapical radiograph demonstrates a well-defined, mixed density entity in relation to #26 and #27, extending from the distal of #26 to distal of #27, measuring approximately 2 cm in its greatest dimension. There is no evidence of root resorption, but there is evidence of loss of lamina dura. Given the ethnicity and presentation, what is your impression?
INCORRECT.
An isolated lesion of osseous dysplasia other than lower anterior in the mandible is termed as focal osseous dysplasia. However, the PA shows a mixed density lesion in the anterior region.
INCORRECT.
The coronal portion of the tooth doesn’t demonstrate any dental caries. The lamina dura and PDL is intact and appears to be in WNL. No apical radiolucency that is correlating to radiographic presentation is noted.
CORRECT.
This lesion has been previously referred to as periapical cementoosseous dysplasia (PCOD). Lack of evidence of cementum on histological examination changed the terminology to periapical osseous dysplasia (POD). POD shows high prevalence in the lower anterior region, with the epicenter being at the apex of the root presenting with the sclerotic border. Vitality test shows teeth Vital. Diagnosis is mostly based on radiographic and clinical characteristics only. Treatment is normally not required. However, radiographic monitoring is recommended.
INCORRECT.
Retained root tip generally reveals PDL space, lamina dura surrounding the left out root tip. Additionally, there is no evidence of pulp canal.
August 2015 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
July 2015
A 25-year-old male reported to the dental clinic for a regular check-up. Clinical examination WNL and radiographic examination revealed a well-defined, radiopaque structure in the upper anterior maxillary region. What is the most likely diagnosis?
INCORRECT.
Complex odontomas appear as an irregular calcified mass (no tooth-like structures are noted) on radiographs and are surrounded by a radiolucent rim.
INCORRECT.
Radiographically, a compound odontoma appears as multiple, tooth-like structures with varying dimensions and these structures are surrounded by a radiolucent rim.
CORRECT.
The supernumerary that occur in between maxillary teeth are called as mesiodens. These teeth are in addition to normal compliment of the teeth and can be identified by counting the teeth. These teeth appear as miniature tooth.
July 2015 References
White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation, 7th Edition, Mosby; 2014
June 2015
35-year-old female presented to the dental clinic with desquamative gingiva and severe ragged erosions on the palate and buccal mucosa. Biopsy of the lesion showed intraepithelial separation, occurring just above the basal cell layer of the epithelium. Direct immunofluorescence examination of tissue submitted in Michel’s solution revealed IgG, IgM and C3 localization in the intercellular spaces between the epithelial cells. What is the most likely diagnosis?
INCORRECT.
Histopathologic feature of mucous membrane pemphigoid shows a split between the surface epithelium and the underlying connective tissue in the region of the basement membrane. Direct immunofluorescence studies of perilesional mucosa show a continuous linear band of immunoreactants (IgG, C3 and occasionally IgA and IgM) at the basement membrane zone in nearly 90% of affected patients.
CORRECT.
INCORRECT.
Subepithelial or intraepithelial vesiculation may be seen in association with necrotic basal keratinocytes with mixed inflammatory infiltrate. Because the immunopathologic features are also nonspecific, the diagnosis is often based on the clinical presentation and the exclusion of other vesiculobullous disorders.
INCORRECT.
Chronic ulcerative stomatitis is similar to those of lichen planus. The diagnosis is essentially based on its characteristic immunopathologic pattern. With direct immunofluorescence studies, autoantibodies (usually IgG) that are directed against the nuclei of stratified squamous epithelial cells in the basal and parabasal regions of the epithelium are detected.
INCORRECT.
The histopathology of lichen planus shows destruction of the basal cell layer of the epithelium, accompanied by an intense, bandlike infiltrate of predominantly T lymphocytes immediately subjacent to the epithelium. The immunopathologic features of lichen planus are nonspecific. Most lesions show the deposition of a shaggy band of fibrinogen at the basement membrane zone.
June 2015 References
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 4th Edition, W.B. Saunders Co.; 2015
May 2015
62-year-old female presented to the dental clinic with burning sensation in the mouth, especially the tongue. Clinically, the tongue exhibited erythroleukoplakic areas where the leukoplakic regions could be rubbed off. What is the most likely diagnosis?
INCORRECT.
Also known as perlèche, it involves the angles of the mouth (angular is characterized by erythema, fissuring, and scaling).
INCORRECT.
Chronic hyperplastic candidiasis is characterized by a white patch that cannot be removed by scraping. Such lesions are usually located on the anterior buccal mucosa and cannot clinically be distinguished from a routine leukoplakia. The diagnosis is confirmed by the presence of candidal hyphae associated with the lesion and by complete resolution of the lesion after antifungal therapy.
INCORRECT.
Also known as “antibiotic sore mouth”, erythematous candidiasis usually follows a course of broad-spectrum antibiotic therapy. Patients often complain that the mouth feels as if a hot beverage had scalded it. This burning sensation is usually accompanied by a diffuse loss of the filiform papillae of the dorsal tongue, resulting in a reddened, “bald” appearance of the tongue.
CORRECT.
Also known as thrush, it is characterized by the presence of adherent white plaques that resemble cottage cheese or curdled milk on the oral mucosa. The white plaques are composed of tangled masses of hyphae, yeasts, desquamated epithelial cells, and debris that can be scraped off. The underlying mucosa may appear normal or erythematous. Antibiotic exposure is typically responsible for an acute (rapid) expression of the condition; immunologic problems usually produce a chronic (slow-onset, long-standing) form.
INCORRECT.
More commonly known as “denture stomatitis”, it is often classified as a form of erythematous candidiasis. This condition is characterized by varying degrees of erythema localized to the denture-bearing areas of a maxillary removable dental prosthesis. The condition is rarely symptomatic. Usually the patient admits to wearing the denture continuously, removing it only periodically to clean it. The denture typically shows much heavier colonization by yeast than the palatal mucosa.
May 2015 References
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 4th Edition, W.B. Saunders Co.; 2015
April 2015
A 25-year-old male presented to the dental clinic with a chief complaint of intermittent soreness in the mouth for several months. The patient has no significant medical history and does not take any medications. Intraoral examination revealed lace-like, white striations on right and left buccal mucosa. The lesion cannot be wiped off. No other findings noted. What is the most likely diagnosis?
INCORRECT.
INCORRECT.
Though allergic contact stomatitis has several clinical features, the patient did not have any history of recent dental restorations or new medicaments.
CORRECT.
It is immunologically mediated mucocutaneous disorder. It occurs in middle-aged patients with female predominance. Skin lesions appear as purple, pruritic, polygonal papules. Reticular type has no symptoms and involves posterior buccal mucosa bilaterally. Other oral mucosal surfaces involved are lateral and dorsal tongue, gingiva, palate and vermillion border. White lesions appear as papules. They can wax and wane. For asymptomatic cases, no treatment required. Topical or systemic corticosteroids recommended for symptomatic patients.
INCORRECT.
Chronic nibbling produces lesions most frequently located on buccal mucosa. It is found in people under stress or psychological conditions. Clinically, it can be bilateral or unilateral. It appears as thickened, shredded, white areas combined with intervening zones of erythema, erosion or focal traumatic ulceration. Areas of white mucosa show irregular ragged surface. Altered mucosa located in mid-portion of anterior buccal mucosa along occlusal plane. No treatment is required.
INCORRECT.
Linea alba is a common alteration of buccal mucosa which is associated with pressure, frictional irritation, sucking trauma from facial surface of teeth. Clinically it appears as white line (usually bilateral) and may be scalloped. It is located on buccal mucosa at level of occlusal plane of adjacent teeth. No treatment is required.
April 2015 References
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 3rd Edition, W.B. Saunders Co.; 2009
March 2015
A 16-year-old male reported to the dental clinic for a regular checkup. Radiographic examination revealed a well-defined, mixed density lesion, and a radiolucent margin in the left mandibular region is noted. The tooth #21 is impacted and a retained deciduous molar is noted as well. What is the most likely diagnosis?
INCORRECT.
A calcifying cystic odontogenic tumor appears as a unilocular, well-defined radiolucency, although the lesion may occasionally appear multilocular. Radiopaque structures within the lesion, either irregular calcifications or toothlike densities can be present as small flecks or smooth pebbles. In some cases, it may be associated with an odontoma.
INCORRECT.
An adenomatoid odontogenic tumor can appear as a circumscribed, unilocular radiolucency that involves the crown of an unerupted tooth or located between the roots of erupted teeth. The lesion is usually completely radiolucent; however, it can contain fine (snowflake) calcifications.
INCORRECT.
Radiographically, a compound odontoma appears as multiple, tooth-like structures with varying dimensions and these structures are surrounded by a radiolucent rim.
CORRECT.
Complex odontomas appear as an irregular calcified mass (no tooth-like structures are noted) on radiographs and are surrounded by a radiolucent rim.
INCORRECT.
Radiographically, a calcifying epithelial odontogenic tumor exhibits either a unilocular or a multilocular radiolucent defect usually associated with an impacted tooth. The margins of the lytic defect are often scalloped and usually relatively well-defined. However, in some cases they exhibit an ill-defined periphery. The lesion may be entirely radiolucent, but the defect usually contains scattered calcified structures of varying size and density. One of the characteristic features is appearance of radiopacities close to the crown of an embedded tooth.
March 2015
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 3rd Edition, W.B. Saunders Co.; 2009
White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation, 7th Edition, Mosby; 2014
February 2015
A 14-year-old male presents to the dental clinic with upper and lower lip swelling present for several days. The patient has noncontributory medical history. The incisional biopsy revealed chronic inflammatory infiltrate with formation of noncaseating granulomas. What is the diagnosis?
INCORRECT.
Angioedema is diffuse edematous swelling of the soft tissues that most commonly involves the subcutaneous and submucosal connective tissues. It is commonly caused by histamine release from mast cells due to presence of allergen.
INCORRECT.
CORRECT.
Orofacial granulomatosis is a term used to describe swelling of the orofacial area, mainly in the lips, due to an underlying granulomatous inflammatory process. It can be an oral manifestation of diseases like sarcoidosis and Crohn’s disease and possibly may be associated with a dietary trigger. It is also commonly seen as a sign of allergic reaction to common food allergens, such as cinnamon and benzoate. The labial tissues demonstrate a nontender, persistent swelling that may involve one or both lips. The diagnosis of orofacial granulomatosis is made on histopathologic demonstration of granulomatous inflammation that is associated with negative special stains for organisms and no foreign material.
INCORRECT.
INCORRECT.
February 2015 References
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 3rd Edition, W.B. Saunders Co.; 2009
January 2015
A 40-year-old female presented to dental clinic with 0.5 x 0.5 cm mucosa colored, sessile gingival nodule. Upon histopathologic examination, the lesion showed bone formation surrounded by fibrous connective tissue. What is your diagnosis?
INCORRECT.
Peripheral odontogenic fibroma is a benign neoplasm of odontogenic ectomesenchymal origin. Histopathologically, it is characterized by relatively mature collagenous fibrous tissue with scattered odontogenic epithelium.
INCORRECT.
INCORRECT.
Peripheral giant cell granuloma represents a reactive lesion, not a true granuloma, caused by local irritation or trauma. Microscopic examination shows a proliferation of multinucleated giant cells. The clinical appearance is similar to pyogenic granuloma, where the peripheral giant cell granuloma often is more blue-purple compared with the bright red of a typical pyogenic granuloma.
CORRECT.
Peripheral ossifying fibroma is a relatively common gingival growth that is considered to be reactive rather than neoplastic in nature. It occurs exclusively on the gingiva. The microscopic pattern of shows fibrous proliferation associated with the formation of a mineralized product. Excision is usually curative; however a recurrence rate of 8% to 16% has been reported.
INCORRECT.
Pyogenic granuloma is a common tumor-like growth considered to be reactive in nature. It is not a true granuloma but a tissue response to local irritation or trauma.
January 2015 References
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 3rd Edition, W.B. Saunders Co.; 2009
December 2014
A 71 y.o. Caucasian male presents to the dental clinic for initial exam. Radiographic examination revealed radiopaque mass with irregular border at mid-posterior portion of right ramus. What is the most likely diagnosis?
INCORRECT.
CORRECT.
Tonsilloliths are discovered on panoramic radiographs as radiopaque objects superimposed on the midportion of the mandibular ramus. Small tonsilloliths are asymptomatic. However, these calcifications can promote recurrent tonsillar infections that may lead to pain, abscess formation, ulceration, dysphagia, chronic sore throat, irritable cough, otalgia, or halitosis. In older adult patients, large tonsilloliths can be aspirated and produce significant secondary pulmonary complications.
INCORRECT.
Benign fibro-osseous lesions, such as osseous dysplasia, present as a radiopaque mass with radiolucent rim and occur in the tooth-bearing region in the jaw.
INCORRECT.
Sialoliths involving parotid gland appear as a round to cylindrical in shape radiopacity and will superimpose on the body of the ramus radiographically.
INCORRECT.
Idiopathic osteosclerosis presents as a focal area of increased radiodensity that is of unknown cause. Radiographically, the lesions are characterized by a well-defined, smooth border, rounded, or elliptic radiodense mass.
December 2014 References
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 3rd Edition, W.B. Saunders Co.; 2009
White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation, 6th Edition, Mosby; 2009
November 2014
An 11-year-old African-American male presented to the pediatric clinic with a red lesion at marginal gingiva of #6. What is the most likely diagnosis?
INCORRECT.
Pyogenic granuloma represents an exuberant tissue response to local irritation or trauma that grows rapidly. In spite of its name, it is not a true granuloma. It is a smooth or lobulated mass that is usually pedunculated. The surface is characteristically ulcerated and ranges from pink to red to purple.
CORRECT.
Localized juvenile spongiotic gingival hyperplasia is characterized by gingival overgrowth as determined by clinical or histopathologic features rather than a pure inflammatory process with minimal to no tissue swelling. The lesion occurs between 5-15 years of age and classically presents as a small, localized, papillary or velvety, bright red, and easily bleeding gingival overgrowth with predilection for facial gingiva. The hyperplasias are confined to attached gingiva, but not all cases involve marginal gingiva.
INCORRECT.
Inflammatory papillary hyperplasia is characterized by reactive tissue growth as a result of ill-fitting maxillary denture or poor denture hygiene. Clinically, the mucosa is erythematous and has a pebbly or papillary surface.
INCORRECT.
Squamous papilloma is a benign proliferation of stratified squamous epithelium which has papillary presentation. The lesion appears as a soft, painless, exophytic lesion with numerous fingerlike projections that can be pointed or blunted.
INCORRECT.
Puberty gingivitis occurs around the time of puberty (period of increased susceptibility to gingivitis). The inflammatory lesion exhibits diffuse involvement of marginal gingiva.
November 2014 References
Chang JY, Kessler HP, Wright JM. “Localized juvenile spongiotic gingival hyperplasia.” Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106, no. 3 (2008): 411-8.
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 3rd Edition, W.B. Saunders Co.; 2009
October 2014
A 55 y.o. African-American male presents to dental clinic for initial visit. Upon radiographic examination, a mixed radiolucent/radiopaque lesion was noted at the apex of #20. The lesion had a radiolucent rim around radiopaque center. Patient was asymptomatic and the tooth was vital. No expansion noted clinically. What is the most likely diagnosis?
INCORRECT.
Idiopathic osteosclerosis presents as a focal area of increased radiodensity that is of unknown cause. Radiographically, the lesions are characterized by a well-defined, rounded, or elliptic radiodense mass without a radiolucent rim.
INCORRECT.
Cementoblastoma is an odontogenic neoplastic process (derived from cementum). Radiographically, the tumor appears as a radiopaque mass that is fused to one or more tooth roots (distorting the lamina dura) and is surrounded by a thin radiolucent rim.
INCORRECT.
Condensing osteitis presents as localized areas of bone sclerosis associated with the apices of teeth with pulpitis or pulpal necrosis. It is associated with a non-vital tooth. Radiographically, the lesion appears as a uniform zone of increased radiodensity adjacent to the apex of a tooth that exhibits a thickened periodontal ligament space or an apical inflammatory lesion. The lesion does not exhibit a radiolucent border.
CORRECT.
Focal osseous dysplasia is a reactive process that occurs in the tooth-bearing (dentulous and edentulous) areas of the jaws and is probably the most common fibro-osseous lesion encountered in clinical practice. Radiographically, the lesion varies from completely radiolucent to densely radiopaque with a thin peripheral radiolucent rim. Mixed radiolucent and radiopaque is the most common pattern seen. The lesion tends to be well defined, but the borders are usually slightly irregular.
INCORRECT.
Osteoblastoma is benign bone tumor. It presents as painful swelling. Radiographically, the osteoblastoma may appear as a well-defined or ill-defined radiolucent lesion often with patchy areas of mineralization.
October 2014 References
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 3rd Edition, W.B. Saunders Co.; 2009
September 2014
A patient presents to the dental clinic with a white, papillary, exophytic lesion on the right anterior portion of the tongue. What is the most likely clinical diagnosis?
CORRECT.
Squamous papilloma is a benign proliferation of stratified squamous epithelium which has papillary presentation. The lesion appears as a soft, painless, exophytic lesion with numerous finger-like projections that can be pointed or blunted (“cauliflower” or wartlike appearance). The lesion is induced by human papilloma virus (low risk HPV 6 and 11 seen in 50% of oral papillomas). The viruses in oral squamous papilloma have extremely low virulence and infectivity rate.
INCORRECT.
Fibroma is the most common reactive lesion of the oral cavity caused because of irritation or trauma. It appears as a smooth-surfaced nodule (sessile or pedunculated) that is similar in color to the surrounding mucosa.
INCORRECT.
Condyloma acuminatum, also known as venereal wart, is a virus-induced proliferation of squamous epithelium of the genitalia, perianal region, mouth, and larynx. Condyloma is considered to be a sexually transmitted disease (STD), with lesions developing at a site of sexual contact or trauma. The typical condyloma appears as a sessile, pink, well-demarcated, non-tender exophytic mass with short, blunted surface projections. The condyloma tends to be larger than the papilloma and is characteristically clustered with other condylomata.
INCORRECT.
Verruca vulgaris, also known as a wart, is a benign, virus-induced, focal epithelial hyperplasia. It is contagious and can spread to other parts of a person’s skin or mucous membranes by way of autoinoculation. It infrequently develops on oral mucosa but is extremely common on the skin. Clinically, it appears as painless, exophytic, papillary lesion that is white in color.
INCORRECT.
Focal epithelial hyperplasia is a virus-induced, localized proliferation of oral squamous epithelium. This disease typically appears as multiple soft, nontender, flattened or rounded papules, which are usually clustered and the color of normal mucosa, although they may be scattered, pale, or rarely white. Occasional lesions show a slight papillary surface change.
September 2014 References
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 3rd Edition, W.B. Saunders Co.; 2009
August 2014
A 13-year-old female presents to the dental clinic for routine care. Upon radiographic examination, a teardrop-shaped, well-defined radiolucency is noted between the right mandibular lateral incisor and canine, causing displacement of teeth. Both teeth were vital. What is the most likely diagnosis?
INCORRECT.
Dentigerous cysts are related exclusively to impacted teeth in coronal position.
INCORRECT.
Lateral radicular cysts appear to be laterally positioned to the tooth mimicking lateral periodontal cysts, however, the associated tooth will be non-vital.
CORRECT.
Lateral periodontal cyst is thought to arise from epithelial rests entrapped in the lateral periodontium of the tooth. The lesion is asymptomatic and found mostly in the region extending from the lateral incisor to second premolar. It appears as a well-defined radiolucency with prominent cortical boundary and round or oval shape. The radiographic differential diagnosis of such lesions includes keratocystic odontogenic tumor (KOT) or radicular cyst (related to non-vital tooth) at foramen of lateral or accessory pulp canal. The treatment includes excisional biopsy or simple enucleation. There is no recurrence.
INCORRECT.
Gingival cyst of adult is the soft tissue counterpart of a lateral periodontal cyst. It usually does not demonstrate any bony involvement.
INCORRECT.
Radicular (periapical) cyst is associated to the root of non-vital tooth.
August 2014 References
White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation, 6th Edition, Mosby; 2009
July 2014
A 77-year-old female presented to the dental clinic for a routine visit. Upon radiographic examination, a linear radiopacity near the spinal column was noted. During extra-oral examination, patient was asymptomatic. What is the most likely diagnosis?
INCORRECT.
CORRECT.
The styloid process is a long cartilaginous bone located on the temporal bone. The muscles and ligaments which have a role in mastication and swallowing are attached to the styloid process. Ossification of stylohyoid ligament can be detected on panoramic radiographs as linear radiopacity extending from posteroinferior aspect of the ramus toward the hyoid bone. Symptoms, such as neck and cervicofacial pain, related to elongated stylohyoid process or ossification of stylohyoid ligament is called Eagle Syndrome. For asymptomatic individuals, no treatment is required. For symptomatic patients, recommended treatment can include steroid or lidocaine injections into tonsillar fossa or amputation of stylohyoid process.
INCORRECT.
INCORRECT.
Arterial calcifications can be seen in facial artery and are less commonly in the carotid artery. Calcified vessels appear as a parallel pair of thin, radiopaque lines that follow the anatomy of the artery (straight or tortuous).
INCORRECT.
Sialolith involving the parotid gland appears as a round to cylindrical in shape radiopacity and will superimpose on the body of the ramus radiographically.
July 2014 References
White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation, 6th Edition, Mosby; 2009
June 2014
A 52-year-old male presents to the dental clinic for an admitting visit. Radiographic examination revealed a dome shaped radiopacity in the right sinus. What is the most likely diagnosis?
INCORRECT.
True sinus mucocele is an accumulation of mucin that is completely encased by epithelial lining. It can occur by trauma (such as sinus surgery) or it can arise from an obstruction of the sinus ostium, thereby blocking normal drainage.
INCORRECT.
Periapical cysts and granuloma cannot be differentiated by radiographic examination alone. Both lesions are related to non-vital tooth and radiographically appear radiolucent with absence of lamina dura at the apical area.
INCORRECT.
Periapical cysts and granuloma cannot be differentiated by radiographic examination alone. Both lesions are related to non-vital tooth and radiographically appear radiolucent with absence of lamina dura at the apical area.
CORRECT.
Antral Pseudocyst is a retention pseudocyst, where the process consists of inflammatory exudate primarily serum. It accumulates under the maxillary sinus mucosa and causes a dome shaped elevation. It is asymptomatic and the patient is usually unaware of the lesion. The lesion does not require treatment because they can resolve spontaneously without any residual effect on antral mucosa.
INCORRECT.
Odontogenic cysts, such as keratocystic odontogenic tumors, displace the floor of the antrum and the border of the cyst becomes coincident with the bony sinus floor.
June 2014 References
Neville B, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 3rd Edition, W.B. Saunders Co.; 2009
White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation, 6th Edition, Mosby; 2009