February 2020
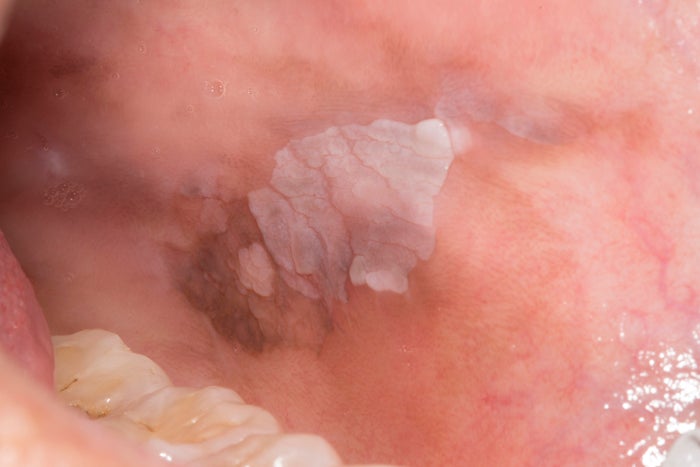
A 59-year-old male patient was referred by his dentist because of a gingival lesion on the lower left side gingiva.
According to the patient, the lesion has been there for 6 months and non-responsive to topical steroid treatment. Buccal gingiva of #20 with a 2 mm buccal defect presents mild edema and erythema with multiple white papules. The patient complained of burning and itchy sensation from the lesion area with an exacerbation when the lesion was irritated by spicy food and flossing. The patient had a medical history of prostate cancer s/p treatment and HIV infection. Both conditions are stable.
CORRECT.
From the clinical appearance of mixed white and red lesion, erythroleukoplakia can be used as a clinical term in this case. Over 90% of erythroleukoplakia represent dysplasia, carcinoma-in-situ, or invasive carcinoma. Gingiva is frequently involved in erythroleukoplakia. Histopathologically, carcinoma in situ was presented in the biopsy.
INCORRECT.
Erosive lichen planus can be presented as red and raw appearance with sensitive or painful areas. However, its lack of response to corticosteroid makes the conventional “lichen planus” unlikely. The histopathology is not consistent with erosive lichen planus.
INCORRECT.
The wright papules and plaques usually can be wiped off and Pseudomembranous candidiasis is often associated with immune dysfunction such as HIV infection or leukemia, medication use such antibiotic, and dry month. However, the white lesion papules cannot be wiped off and no candidal hyphae or spores could be found histopathologically.
February 2020 References
Wetzel SL, Wollenberg J. Oral Potentially Malignant Disorders. Dent Clin North Am. 2020;64(1):25-37.
January 2020
A 66-year old male patient was referred for multiple mucosal lesions on the tongue. The lesions were noticed by his dentist recently in a routine examination.
A fissured and erythematous area with a slightly elevated white linear border is observed on both sides of the lateral tongue. A similar erythematous lesion with a white border can also be found on the left side of the ventral tongue. The patient’s past medical history includes hypertension and high cholesterol and was on Aspirin, Amlodipine, and Benazepril. The patient smoked 1 pack/day for 1 year only and was a social drinker.
INCORRECT.
Candidiasis can also present with tongue papillary atrophy and/or with psoriasiform epithelial hyperplasia, which could lead it to be one of the differential diagnosis in this case. The fissured tongue can also increase the risk for candidiasis infection. However, in this case, no candidal hyphae or spores were found histopathologically.
INCORRECT.
Considering the patient’s age and tobacco use history, Erytholeukoplakia could be considered as one of the possibilities of the clinical diagnosis. The lesion on the left ventral tongue showed red patch with surrounded white border may be more suspicious. A biopsy was done to rule out as no epithelial dysplasia was found histopathologically.
CORRECT.
Erythema migrans primarily affects the tongue with an unclear etiopathogenesis.The erythema is usually caused by the atrophy of the filiform papillae and a slightly elevated, yellow-white border could be seen around or partially around the erythema.1/4-1/3 of patients also present fissured tongue.The lesions are commonly asymptomatic Histopathological finding includes hyper parakeratosis, acanthosis, and infiltration of inflammatory cell involved in the lamina propria, which is consistent with the diagnosis of psoriasiform mucositis.
January 2020 References
Banakar M. What are the best treatments for benign migratory glossitis? Evid Based Dent. 2019;20(2):40-41.
McNamara KK, Kalmar JR. Erythematous and Vascular Oral Mucosal Lesions: A Clinicopathologic Review of Red Entities. Head Neck Pathol. 2019;13(1):4-15
October 2016
A 47-year-old male was referred to the Department of Oral & Maxillofacial Medicine and Diagnostic Sciences to acquire a panoramic image. No significant medical history was elicited during clinical examination. The panoramic radiograph showed a well-defined radiolucent region in the left mandibular region. The lesion is curvilinear in shape and measures approximately 11.13 mm x 9.03 mm in its greatest dimensions. The internal content is homogeneous, radiolucent in nature. No bony reaction noted. Identify the abnormality (green arrows) and provide your diagnosis.
INCORRECT.
Ossifying fibroma (OF) affects middle-aged females and is more predominant in the premolar-molar area. It is usually described as a mixed density lesion with concentric expansion of the cortical plate. Lack of these radiographic features precludes this entity.
CORRECT.
SBD is asymptomatic and may be noted as an incidental finding in routine dental imaging.
It is relatively easy to diagnose, especially if typical radiographic features are present. These features include a round to oval radiolucent region with an intact cortical bone. The location is another key factor for diagnosis; SBD is located below IAC and near the angle of the mandible. The radiographic impression should suffice the diagnosis and this should preclude any surgical exploration. Radiographic follow-up is recommended.
INCORRECT.
Residual cysts occur as a result of incomplete removal of radicular or other inflammatory cyst. The location is pathognomonic for this lesion, i.e. they tend occur in the edentulous ridge and are usually located above the inferior alveolar canal (IAC). This panoramic view shows the lesion to be below the IAC.
October 2016 References
White, Stuart C., and Michael J. Pharoah. Oral Radiology: Principles and Interpretation, 7th Edition. Mosby, 2014. VitalBook file.
September 2016
A 55-year-old female presents with an asymptomatic, solitary white lesion of the left buccal mucosa. The patient had been unaware of its presence. The patient’s medical history is non-contributory and she does not take any medications. What is the most likely diagnosis?
INCORRECT.
Chronic nibbling produces lesions most frequently located on the buccal mucosa. It may be found in people under stress, but also in patients entirely unaware of their parafunctional habit. Clinically, it can be bilateral or unilateral. It appears as thickened, shredded, white areas combined with intervening zones of erythema, erosion or focal traumatic ulceration. Areas of white mucosa show an irregular ragged surface. The altered mucosa is located in the mid-portion of the anterior buccal mucosa along the occlusal plane. No treatment is required.
CORRECT.
Leukoplakia is the most common precursor lesion to squamous cell carcinoma of the oral cavity. There is a male predilection, presumably due to the commonly implicated risk factors, smoking and alcohol. It presents as a white plaque with generally well-demarcated borders. Early lesions present as homogenously smooth and thin, and more advanced lesions may present with nodular, verrucous, or even partially erythematous components (erythroplakia). The area of hyperpigmentation located posteriorly may represent a coexisting melanotic macule or an unusual example of post-inflammatory hyperpigmentation (PIH), which is most characteristically associated with lichen planus.
INCORRECT.
Lichen planus is an immunologically mediated mucocutaneous disorder. It tends to occur in middle-aged patients with female predominance. Skin lesions appear as purple, pruritic, polygonal papules. Oral lesions may be white, red, or ulcerative. The reticular type presents with classic Wickham striae, typically on the posterior buccal mucosa bilaterally, and is frequently asymptomatic. Other common surfaces involved are the ventrolateral tongue and the gingiva. Erythematous and ulcerative presentations may be symptomatic. For asymptomatic cases, no treatment is required. Topical or systemic corticosteroids are recommended for symptomatic patients. Disease course is variable but my be waxing or waning.
September 2016 References
Neville BW, Damm DD, Chi AC, Allen CM. Oral and maxillofacial pathology. Elsevier Health Sciences; 2015.
Greenberg MS, Glick M (2003). Burket's oral medicine diagnosis & treatment (10th ed.). Hamilton, Ont.: BC Decker. pp. 87,88,90–93,101–105. ISBN 1-55009-186-7.
Thongprasom, K; Carrozzo, M; Furness, S; Lodi, G (Jul 6, 2011). Interventions for treating oral lichen planus. The Cochrane database of systematic reviews (7): CD001168. doi:10.1002/14651858.CD001168.pub2. PMID 21735381.