With Moderna Inc. global fellowship award, CWRU School of Medicine researchers hope to develop process that overcomes challenge of targeting diseased cells
Beyond vaccines, mRNA offers immense potential to fight disease, but targeting the genetic material to specific diseased cells is challenging—requiring a new method.
To meet this need, researchers at Case Western Reserve University School of Medicine, with a Global Research Fellowship award from Moderna Inc., are developing a process that essentially uses bubbles to overcome the problem.
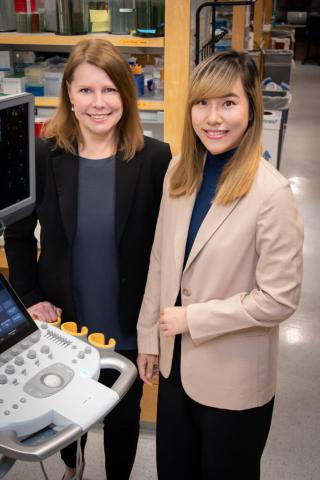
“If these challenges can be overcome, this approach could lead to new and more effective ways of delivering therapies to specific cells in the body,” said Agata Exner, the Henry Willson Payne Professor and vice chair for basic research in the Department of Radiology at the School of Medicine, who is leading the research. “This could be especially important in treating diseases like cancer or genetic disorders, where specific cells need to be targeted without harming healthy cells.”
Moderna, a leading COVID-19 vaccine producer, recently awarded postdoctoral scholar Pinunta “Petch” Nittayacharn in the Exner lab the fellowship for their work in the drugmaker’s inaugural round of research grants.
Messenger ribonucleic acid—mRNA for short—is a genetic material that tells the body how to make protein. Vaccines, like Moderna’s COVID-19 vaccine, use mRNA that, when injected, triggers an immune response inside the body. The immune response produces antibodies that protect people from illness.
To take mRNA’s disease-fighting effectiveness even further, Exner and Nittayacharn are working to develop a more efficient way to deliver the material into targeted cells using tiny gas-core particles—called nanobubbles (NBs)—with a targeting molecule to deliver the mRNA into specific cells.
When combined with noninvasive, gentle sound waves that can be used without harming the body, the NBs can make it easier to enter cells by “cavitation,” or popping the bubbles, resulting in more efficient gene delivery, Nittayacharn said.
The approach has been tried with larger microbubbles, but the particles were too big to escape the blood vessel and move into the surrounding tissue, the researchers said. But NBs are 1,000 times smaller and can escape from leaky blood vessels in diseases—such as tumors—and accumulate in the targeted tissue.
“Of course, there are still many challenges and potential limitations to this approach that will need to be addressed, such as optimizing the design of the NBs, ensuring that the mRNA is effectively released from the NBs once inside the cell and minimizing any potential toxicity or immune reactions,” Exner said. “The future of mRNA delivery will be shaped by this, and many other approaches being developed in research labs worldwide.”
For more information, contact Bill Lubinger at william.lubinger@case.edu.
This article was originally published April 11, 2023.