Scientists have determined that fungus may play a key role in chronic intestinal inflammation disorders. They found that patients with Crohn’s disease tend to have much higher levels of the fungus Candida tropicaliscompared to their healthy family members. A new review published in Digestive and Liver Disease looks at these findings and provides insights into potential new therapeutic approaches using antifungals and probiotics in the treatment of inflammatory bowel diseases (IBD) such as Crohn’s disease (CD).
“The human gastrointestinal (GI) tract is home to trillions of microorganisms, some beneficial and others potentially harmful. Recent advances in science have allowed us to identify the multitude of organisms inhabiting the GI tract and parse out those that play a role in IBD,” explained lead author Mahmoud A. Ghannoum, PhD, of the Center for Medical Mycology, Department of Dermatology, Case Western Reserve University and, University Hospitals Cleveland Medical Center, Cleveland, OH. “Unfortunately, most research has focused on studying only the bacteria while overlooking a key player, fungus. In order to address this issue, we have focused our efforts on studying the fungal community in the GI tract known as the mycobiome.”
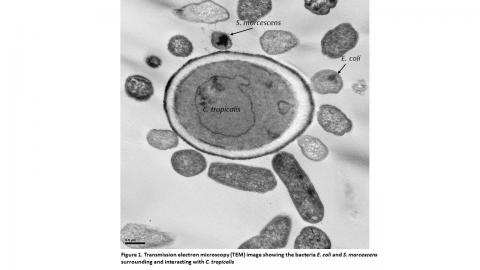
The review centers on a first of its kind study in which researchers characterized the gut bacterial microbiota (bacteriome) and fungal community (mycobiome) in a number of families that had members with CD and healthy relatives. They then defined the microbial interactions leading to microbial imbalance in the family members suffering from CD. They found that family members with CD had fungal (Candida tropicalis) and bacterial (Serratia marcescens and Escherichia coli) imbalances in their gut’s microbiome. Interestingly, they showed that these three organisms worked together to form robust digestive plaque biofilms capable of exacerbating intestinal inflammation.
Although the relationship between bacteria and fungi has been recognized not only in our gut, but in our body at large, this study proved for the first time that bacteria and fungi actually work together to exacerbate the inflammatory symptoms in CD. These results provide insight into the roles of bacteria and fungi in CD and may lead to the development of novel treatment approaches and diagnostic tests for CD and other debilitating digestive issues.
Promising potential treatments could include using antifungals and even probiotics that are designed to balance both bacteria and fungi, while breaking down digestive plaque biofilms. Antifungals will control the overgrowth of fungi, while probiotics can help restore and maintain the balance of the microbiota, noted the authors.
“Our ground-breaking discovery that bacteria and fungi both play a critical role in health and disease has tremendous implications not only for understanding the disease process, but also for development of potentially life changing treatments for those who suffer from chronic digestive diseases,” concluded Dr Ghannoum.
For more information about Case Western Reserve University School of Medicine, please visit: case.edu/medicine.
Media Contact(s):
Marc Kaplan
Associate Dean, Marketing & Communications
Case Western Reserve University School of Medicine
Office: 216-368-4692
Marc.Kaplan@case.edu
Ansley Gogol
Associate Communications Specialist
Case Western Reserve University School of Medicine
Office: 216-368-4452
Ansley.Gogol@case.edu