Funding supports newly published findings showing some medications trigger ‘cell blasters’ to kill cancer
With a new $2 million federal grant, a researcher at Case Western Reserve University School of Medicine will lead a team to further explore preliminary findings of an effective treatment for colorectal and possibly other cancers.
The grant, from the National Institutes of Health’s National Cancer Institute, supports the team’s promising results recently published in The Journal of Clinical Investigation.
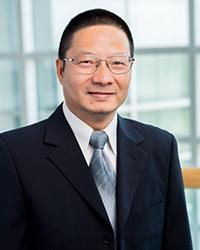
“We reported a novel discovery that some cancer medications trigger ‘cell blasters’ to kill cancer,” said Zhenghe “John” Wang, the Dale Cowan–Ruth Goodman Blum Professor of Cancer Research and chair of the Department of Genetics and Genome Sciences at the School of Medicine.
Wang is also co-leader of the Cancer Genomics and Epigenomics Program at the Case Comprehensive Cancer Center (Case CCC).
Case CCC members David Bajor, an assistant professor at the School of Medicine and an oncologist at University Hospitals, and Alok Khorana, a professor at the School of Medicine and the Sondra and Stephen Hardis Chair in Oncology Research at Cleveland Clinic, are Wang’s collaborators on a clinical trial to test a new cancer treatment.
Their findings
White blood cells are the immune system’s first line of defense against bacterial infection. Neutrophils, the most abundant white blood cells, can undergo a self-destructive process to release web-like structures—called “neutrophil extracellular traps,” or NETs—to trap and kill bacteria, Wang explained.
In their study, the researchers found that combining two chemotherapy drugs (CB-839 and 5-FU) stopped the growth of a type of colon cancer in mouse models that involves PIK3CA—a gene that controls cell growth. They credited the success partly on NETs, because the drugs weren’t as effective when the traps were disturbed.
“We found that patients with tumors that have increased amounts of NETs after the drug treatment survived longer,” Wang said. “We found that certain cancer drugs hijack these neutrophils to kill cancers using extracellular traps. So, our study reveals a new way cancer drugs work, paving the way for the design of new cancer treatments.”
The study could have a broader impact beyond colorectal cancer, Wang said, because PIK3CA is mutated in about 20% of all human cancers. The mechanisms identified in the study also may apply to other NET-related diseases, he said.
The next steps, he said, are to understand how chemotherapies modulate NET production and then use what they learn to design novel cancer treatments.
For more information, contact Bill Lubinger at william.lubinger@case.edu.
This article was originally published Feb. 8, 2024.